An Unexpected Twist in Spinal Surgery: An Opinion Editorial
The world of modern spinal surgery is constantly evolving, but, with every advancement comes a series of tricky parts and tangled issues that demand our constant attention. Recently, a particularly nerve-racking case involving the migration of a Nelaton catheter cover into the pulmonary artery during lumbar disc surgery has caught the professional community’s eye. This incident, though rare, sheds light on the hidden complexities of using improvised tools during surgery and offers valuable lessons for surgeons, medical teams, and hospital administrators alike.
This editorial aims to take a closer look at the case, explore the tangled issues it reveals about improvised surgical practices, and spark a conversation about rethinking essential safety protocols in spinal procedures. In doing so, we will examine the detailed nitty-gritty of this case report, evaluate how such events happen, and discuss strategies to better manage such situations in the future.
Learning from an Unforeseen Surgical Complication
In the case in question, a 71‐year‐old man with a history of diabetes mellitus and lumbar disc herniation underwent a posterior lumbar decompression and fusion procedure at the L5/S1 level. As he reported lower back discomfort, leg numbness, and pain that restricted his daily activities, the planned surgical intervention aimed to alleviate these symptoms and improve his quality of life.
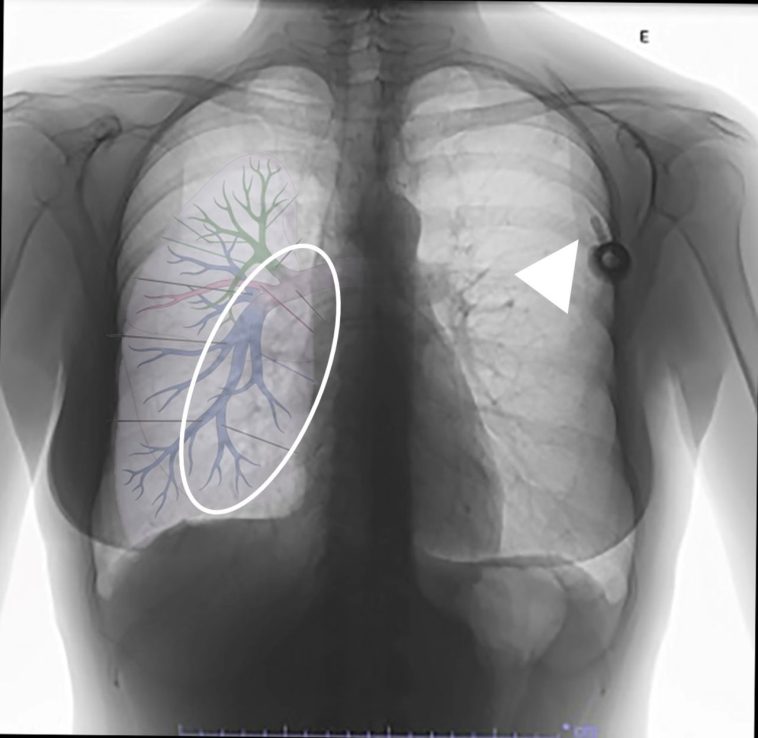
During the operation, a common iliac vein injury emerged as a result of the disc curettage process—a step that, under normal circumstances, requires precise handling and careful judgement. In an effort to control the bleeding from a small venous tear, a suction tube enhanced with a Nelaton cover was employed. This makeshift device, typically used to protect suction tips from high-speed drills, ultimately became dislodged. It then migrated through the vascular system, resulting in a pulmonary artery embolism that required immediate surgical removal by a team of thoracic surgeons.
Such an event, while undeniably alarming, also serves as an essential case study for understanding how improvisation in the operating room, when not managed with foolproof safety measures, can lead to dangerous outcomes. It forces us to re-examine the established methods and question the reliance on unconventional practices that may, at times, be off-putting in their application.
Risks of Improvised Surgical Hemostasis Tools
One of the most intriguing aspects of this case is the use of a Nelaton catheter cover—a tool originally intended for urological procedures—to serve as an extra layer for hemostasis during disc curettage. Although this practice aims to protect the suction tube from potential damage caused by a high-speed drill, it inadvertently introduces a potential vector for complications when not correctly secured.
Safety Concerns When Using Non-Standard Tools
Using improvised devices in surgery is not uncommon; however, it is essential to weigh the benefits against the risks. The following bullet list outlines the key safety concerns associated with the use of such non-standard tools:
- Detachment Risk: The small, flexible segment of the Nelaton catheter, when not secured adequately, can easily detach during critical moments of surgery.
- Migration Hazard: Once detached, this piece can travel through the body’s vascular system, posing a serious embolism risk as it can lodge in major vessels like the pulmonary artery.
- Lack of Standardization: There are no universally established guidelines or protocols for the use of a Nelaton cover in spinal procedures, which opens the door for varying practices and potential mismanagement.
- Unintended Tissue Injury: The use of these improvised tools may introduce additional manipulative steps during an already complex procedure, increasing the risk of further tissue or vascular injury.
These concerns are not meant to discourage any innovative measures that can improve surgical outcomes; rather, they underline the importance of establishing strict, standardized protocols to ensure that such tools enhance rather than jeopardize patient safety.
Comparing Traditional and Improvised Techniques
The differences between conventional and improvised methods in surgical procedures often boil down to predictability and control. Traditional hemostatic methods have undergone rigorous evaluation over time, while improvised techniques can be full of problems not immediately evident until complications arise. A table comparing these two approaches may provide a clear understanding:
| Parameter | Traditional Methods | Improvised Techniques |
|---|---|---|
| Safety Profile | Well-documented and standardised | Potentially inconsistent and risky |
| Predictability | High, with established protocols | Low, with unpredictable outcomes |
| Training and Familiarity | Widely taught and practiced | May require additional on-the-spot judgment |
| Regulation and Monitoring | Strict guidelines in place | Often lacks rigorous standardization |
This comparison illustrates that even though improvised solutions may be attractive in dire situations, their unpredictable nature makes them a nerve-racking choice when it comes to patient safety.
Understanding How Instrument Detachment Occurs
Instrument detachment in the operating room is one of the more complicated pieces of the challenges faced by surgical teams. In the case of the detached Nelaton cover, several factors contributed to this unsettling event:
- Force and Pressure Applied: The lateral approach used during disc curettage may have required a deeper insertion of surgical tools, accidentally exerting additional pressure on the device.
- Unintentional Tissue Interaction: When the forceps grab tissues or when bleeding is encountered, even slight interactions with the vessel wall could dislodge loosely secured equipment.
- Saline Irrigation and Curettage: The flushing and cleaning procedures common in spinal surgery, while essential, can inadvertently aid the migration of unsecured pieces if they enter the vascular system.
Each of these factors highlights the ways in which even well-intentioned safety measures can be undermined when multiple forces and actions combine. A closer look at these details encourages us to get into the broader discussion of ensuring instrument security throughout spinal procedures.
Ensuring Secure Device Attachment During Surgery
To reduce the risk of such nerve-wracking complications, several strategies must be rigorously implemented. Preoperative planning and intraoperative vigilance are key elements that ensure the transient use of devices like the Nelaton cover does not evolve into a major problem.
Meticulous Preoperative Planning and Verification
The first substantial step is thorough preoperative planning. This involves not only mapping out the surgical field using modern imaging techniques such as MRI and CT scans but also setting specific parameters for tool insertion. Surgeons can benefit from:
- Defining Safe Insertion Depths: Establishing critical limits before starting disc curettage can help avoid breaches in the anterior longitudinal ligament and reduce vascular injury risk.
- Double-Checking Attachment Security: Both the scrub nurse and the surgeon should verify that improvised tool attachments, like the Nelaton cover, are securely fastened before the procedure begins.
- Team Briefings: A preoperative discussion that outlines all potential risks and the corresponding strategies can prepare the entire surgical team, making it easier to spot and respond to any problems.
These steps are key to ensuring that even if unexpected pressure or twisting forces occur during the operation, the risk of device detachment is minimized.
Intraoperative Monitoring and Communication
During surgery, managing your way through potential complications requires a well-coordinated team effort. The operating room should have a protocol for intraoperative imaging, especially when any equipment goes missing or when outcomes do not align with expectations. Some recommendations include:
- Immediate Imaging Upon Suspicion: Should any component go unaccounted for, a quick radiographic or fluoroscopic check can help locate it before it migrates to a more critical area.
- Real-Time Team Communication: Maintaining clear and continuous communication between the surgical, anesthetic, and nursing teams ensures that any unexpected twist is swiftly addressed.
- Implementing a Checklist System: Using a detailed checklist that includes verifying all equipment post-procedure can significantly cut down the chances of missing tools or attachments.
These simple yet essential practices are super important to ensure that time-sensitive complications, like a detached device, are managed correctly.
Risks of Vascular Injury in Lumbar Procedures
Vascular injury during lumbar surgery is a full-of-problems domain. Although such injuries are rare, they are laden with the potential for serious, sometimes overwhelming, consequences. Recognizing the dangerous proximity of major blood vessels such as the common iliac vein and the aorta is fundamental to understanding these risks.
Close Proximity of Vital Vessels
Surgical interventions at the L5/S1 level encounter the close vicinity of the common iliac artery, the common iliac vein, and even the aorta. This proximity means that even minor unintentional movements or increased pressure during the procedure can result in significant vascular damage. The following points highlight why this region is particularly risky:
- Vessel Fragility: Vessels in the lumbar area are typically more vulnerable to damage during aggressive surgical maneuvers.
- Anatomical Variations: Variations in the anatomy of blood vessels can complicate the surgical approach, meaning that what works safely for one patient may not be as effective for another.
- Force Distribution: The force applied during curettage, if not evenly distributed, has a higher chance of breaching the vessel walls.
It is these subtle details and fine shades of difference in anatomical structure that demand every surgeon’s utmost care to avoid inadvertent injury.
Complications Arising from Vascular Injuries
The complications that arise from vascular injuries during lumbar surgery are not limited to severe blood loss. They can also include thromboembolic events such as deep vein thrombosis and pulmonary embolism. Some examples of related complications include:
- Hemorrhage: Significant bleeding due to vessel laceration may require rapid intervention.
- Clot Formation: When a blood vessel is compromised, there is potential for the development of clots that can migrate and cause additional issues.
- Organ Damage: In cases where emboli travel to the lungs, respiratory function can be impaired, necessitating further surgical intervention.
- Neurological Sequelae: Vascular injury may also indirectly affect nerve tissues, leading to prolonged recovery or additional surgeries.
Ensuring that each of these risks is evaluated and mitigated during the planning and execution of surgeries is an essential step toward better patient outcomes.
Strategies to Prevent Adverse Outcomes in Spinal Surgery
Every surgical case, particularly those as intricate as spinal fusion, comes with its own set of challenges. However, every challenge, no matter how intimidating it seems, can be managed effectively by implementing strict, evidence-based guidelines. Here, we outline strategies designed to reduce the risk of complications linked to both vascular injury and improvised instrument use.
Enhanced Preoperative Assessment and Simulation
Before stepping into the operating room, thorough assessment and simulation of the operative procedure can help figure a path through potentially risky maneuvers. Key suggestions include:
- Detailed Imaging and Mapping: Leveraging advanced imaging technology (such as high-resolution MRI and CT scans) to identify the exact position and condition of the surrounding vascular structures is critical. Surgeons should use these scans to establish “no-go” zones in the operative area.
- Virtual Simulation: Using surgical simulation software can help medical teams practice the procedure and identify potential pitfalls, benefiting from a simulated environment where errors can be safely studied.
- Risk Stratification: Based on the imaging and clinical history of the patient, a preoperative risk assessment should be carried out. This step ensures that the entire team is aware of and prepared for even the smallest twist in the operating room.
Simulation and preoperative planning are essential to avoid the pitfalls of relying solely on improvisational techniques during a critical procedure. When everyone knows the plan, and every possible scenario is anticipated, the chances of mishaps drop significantly.
Development of Standardized Protocols for Improvised Tool Use
Despite the challenges associated with the use of tools like the Nelaton cover, innovation in the operating room should not be stifled. Instead, it is a call to develop standardized protocols that take into account both safety and efficacy. Such protocols might include:
- Clear Guidelines for Attachment: Establishing a uniform procedure for securely affixing a protective cover to a suction tube can reduce the risk of detachment. This should involve specific measurements, attachment techniques, and methods for double-checking the integrity of the connection.
- Training Workshops: Regular training sessions can be organized for surgical teams, highlighting the proper use of improvised devices and identifying red flags that suggest their retraction.
- Post-Procedure Verification: Incorporating a mandatory check after each surgical step—especially after the use of an improvised device—is essential. This can include immediate imaging for verification if any instrument seems to be out of place.
The introduction of these standardized practices can help ensure that every member of the surgical team is on the same page, reducing the potential for miscommunication and mishandling that ultimately affect the patient.
Teamwork and Communication: The Cornerstones of Safe Surgery
An equally important lesson from this case is the critical role of teamwork and communication. In the operating room, every moment of distraction or miscommunication can lead to a series of small, yet significant, oversights during a procedure.
Effective Intraoperative Communication Techniques
With many moving parts and various teams involved simultaneously, it is super important to ensure clear channels of communication throughout the surgery. Some tried and tested techniques include:
- Pre-Surgical Briefings: Before starting the procedure, a comprehensive briefing should outline every team member’s responsibilities and the potential pitfalls that may occur.
- Real-Time Feedback: Surgeons should encourage immediate feedback from nurses and anesthesiologists, particularly if any unusual movement or instrument behavior is observed.
- Standardized Communication Protocols: Adoption of protocols such as the “closed-loop communication” method can help confirm that every instruction is clearly understood and executed correctly.
When every team member is actively engaged and aware of what to monitor, even the slightest irregularity—such as an instrument slipping or being missing—can be spotted and addressed promptly.
The Role of Checklists in the Operating Room
One practical tool that has been shown to mitigate many mistakes in healthcare is the use of checklists. The surgical checklist is a simple yet effective method to make sure that no critical step is missed. Essential checklist items might include:
- Verification of instrument count before and after the procedure
- Securing all additional devices and improvised attachments
- Prompt imaging if any tool or cover goes missing during the operation
- A formal debrief after surgery to discuss what went well and what could be improved
By integrating these checklists into standard operating protocols, teams can better prepare for the unexpected and efficiently manage the small twists and turns of an already challenging procedure.
The Broader Implications for Healthcare Policy and Practice
This case not only highlights specific technical challenges in spinal surgery but also invites a broader discussion about healthcare policy and the adoption of best practices in surgical environments. As medicine continues to innovate, regulatory bodies and hospital administrations have an essential role to play in ensuring that any new or improvised methods are scrutinized and standardized before becoming widespread.
Establishing Best Practices in Surgical Innovation
Healthcare policy makers can take a proactive approach by encouraging systematic research into the safety and efficacy of improvised devices, such as the Nelaton cover when used outside its typical settings. The following measures could contribute to more secure practice:
- Clinical Trials and Studies: Funding and supporting research that specifically evaluates the use of novel or adapted equipment in surgery can provide data to guide future practices.
- Interdisciplinary Collaboration: Forming committees that include surgeons, biomedical engineers, and patient safety experts can help develop standardized protocols that safely integrate innovation in surgery.
- Regulatory Oversight: Implementing strict regulatory standards for the use of any non-standard surgical devices can minimize variability in practice and enhance patient safety.
When healthcare leaders take these steps, they pave the way for a more consistent surgical environment where innovation and patient safety go hand in hand.
Improving Patient Education and Informed Consent
While much of the focus in this case has been on surgical technique and intraoperative management, it is also crucial to consider the patient’s role in the process. Comprehensive patient education and clear informed consent procedures are essential for maintaining trust and ensuring that patients understand every potential risk even when innovative techniques are used. Guidelines to consider include:
- Transparent Risk Communication: Patients should be informed of the specific risks associated with any improvised technique or new technology being used during surgery.
- Clear Explanations of Procedure: Using clear language and visual aids, surgeons can ensure that patients understand the step-by-step mechanics of the planned intervention.
- Postoperative Expectations: Explaining what patients should monitor and report in the postoperative period can help in early identification of complications.
By taking a proactive approach to patient education, medical professionals can help ensure that patients are more involved in their care and more prepared to face any unforeseen issues.
Maintaining a Culture of Continuous Learning and Improvement
The unexpected complications discussed here serve as a stark reminder that medicine is full of twists and turns. The experience gained from each regrettable event must be used as a springboard for continuous learning and operational improvement. Hospitals and surgical centers should view such incidents as opportunities to analyze, discuss, and ultimately evolve surgical practice for better outcomes.
Postoperative Analysis and Quality Improvement
Successful management of any surgical complication does not end once the procedure is over. A comprehensive, systematic review of every case is essential. Some core components of effective postoperative analysis include:
- Root Cause Analysis: Conducting an in-depth analysis of what precisely went wrong—whether it be device detachment, miscommunication, or procedural misjudgment—can be critical for future prevention.
- Team Debriefings: Bringing together the surgical team after the operation to discuss the event allows each member to share their experiences and propose improvements.
- Documentation and Reporting: Detailed documentation helps in tracking incidents over time and is essential for building a knowledge base that can inform policy and practice.
This culture of open dialogue and continuous learning not only helps in mitigating the risk of similar complications but also bolsters overall team morale and confidence in handling challenging situations.
Embracing Technological Innovations for Safety
As medical technology continues to advance, there is great potential in using tools and systems designed to support surgical teams. Some promising approaches include:
- Real-Time Imaging Technologies: Advancements such as intraoperative CT or 3D imaging can help identify subtle details that might be missed with traditional methods.
- Smart Surgical Instruments: The development of instruments integrated with sensors to monitor attachment security and movement can provide early alerts if a device is at risk of detaching.
- Digital Checklists and AI Support: Utilizing digital platforms and artificial intelligence to monitor adherence to checklists can help in catching mistakes before they escalate mid-procedure.
Investing in these technological improvements is a super important step toward making surgery as safe as possible in the modern era, ensuring that even improvised methods are backed up by robust safety features.
Reflections on That Unsettling Case: The Balance Between Innovation and Safety
Looking back at the complicated pieces of the case involving the dislodged Nelaton cover, it is clear that the incident was not just a mere lapse in procedure; it was an event that unveiled multiple layers of risk inherent in certain surgical practices. The case forces us to take a closer look at the idea that innovation should never override patient safety. Instead, every innovative step must be anchored by rigorous protocols and thorough testing.
This case is a reminder that every new method, even when it promises improved efficiency or convenience, must be examined through the lens of potential risks. It underscores the importance of balancing the desire to workaround a problem with the necessity of ensuring that these solutions do not introduce additional, unintended hazards.
Learning from Past Mistakes to Forge a Safer Future
In reflecting on this case, several lessons emerge that should guide both current practice and future research:
- Be Wary of Improvised Tools: Even if improvisation can lead to short-term solutions, it is critical that every such tool is validated in a controlled setting before it becomes a staple of surgical practice.
- Prioritize Instrument Security: Small slips—like a Nelaton cover detaching—can cascade into full-blown complications that might endanger the patient’s life. Secure attachment must thereby be a non-negotiable element of every procedure.
- Invest in Teamwork Training: The need for clear communication cannot be overstated. Every unsaid detail or unchecked step increases the risk of an inadvertent error.
- Foster a Learning Environment: Establish a culture where every near-miss or adverse event is documented, reviewed, and used as a stepping stone for improving surgical safety standards.
These takeaways should not serve to cast a shadow over the innovations that are driving modern medicine forward. Instead, they reinforce that in the quest for advanced techniques, the patient’s safety should always remain at the forefront.
Conclusion: A Call for Cautious Innovation in Spinal Surgery
The unexpected migration of a Nelaton catheter cover during a lumbar surgery is a stark reminder that the realm of spinal surgery is full of hidden complexities and challenging bits. While innovation and improvisation can be key drivers in improving patient care, they must not come at the expense of safety. Instead, these advances need to be tempered with meticulous planning, solid teamwork, and innovation that is critically scrutinized and standardized before widespread adoption.
For surgeons and healthcare professionals, this case study offers a sobering lesson: every time you take a risk with an improvised tool or a non-standard procedure, you are stepping into a territory loaded with issues that can have dire outcomes if not carefully managed. Preoperative planning, real-time imaging, standardized tool attachment protocols, and a culture that values continuous learning are all super important components of ensuring patient safety in spinal procedures.
As we look ahead, it is essential that the medical community continues to get into and explore the fine points of each case. By systematically addressing and resolving these occasional yet disappointing incidents, we can considerably enhance surgical outcomes and patient satisfaction. This balancing act between innovation and safety is a challenging ride, but it is necessary for ensuring that spinal surgery remains both advanced and secure.
Ultimately, every surgical team is tasked with the dual responsibility of harnessing modern technology to improve patient outcomes while also safeguarding those patients against unintended complications. The lessons learned from this case are not meant to discourage breakthrough innovation; rather, they call for a measured approach where caution is as much a part of the routine as is the step-by-step execution of a once advanced procedure.
By embracing rigorous protocols, fostering clear intraoperative communication, and continuously investing in both human and technological resources, we can steer through the conflicting pressures of innovation and patient safety. It is through such measured and collaborative efforts that the field of spinal surgery can continue to evolve—ensuring that even the most nerve-racking incidents become valuable educational tools, ultimately paving the way for safer, more reliable practices in the future.
This regrettable case of a catheter cover migration may have been a series of unfortunate events, but it also serves as a super important catalyst for change. It reminds us to remain vigilant, rely on proven safety measures, and always prioritize the welfare of our patients over even the most alluring shortcuts. The road ahead may be full of complicated pieces and tricky parts, but with constant attention and a cautious spirit, we can collectively build a safer surgical environment for everyone.
Originally Post From https://www.cureus.com/articles/383873-migration-of-a-nelaton-catheter-into-the-pulmonary-artery-during-spinal-surgery-requiring-surgical-removal-a-regrettable-case
Read more about this topic at
Iatrogenic air embolism: pathoanatomy …
Iatrogenic air embolism: pathoanatomy …