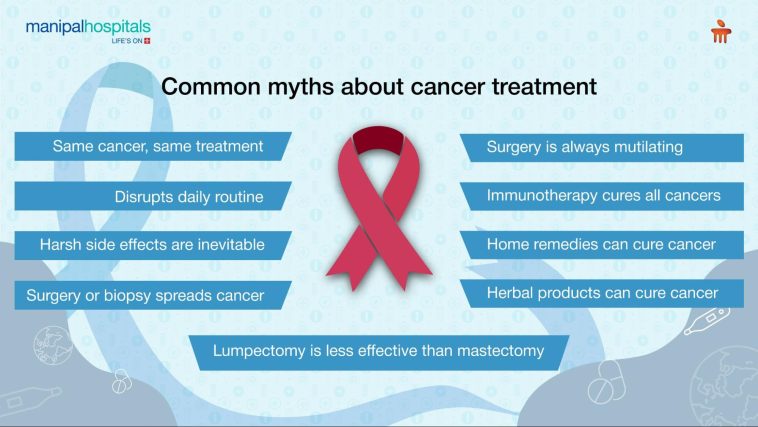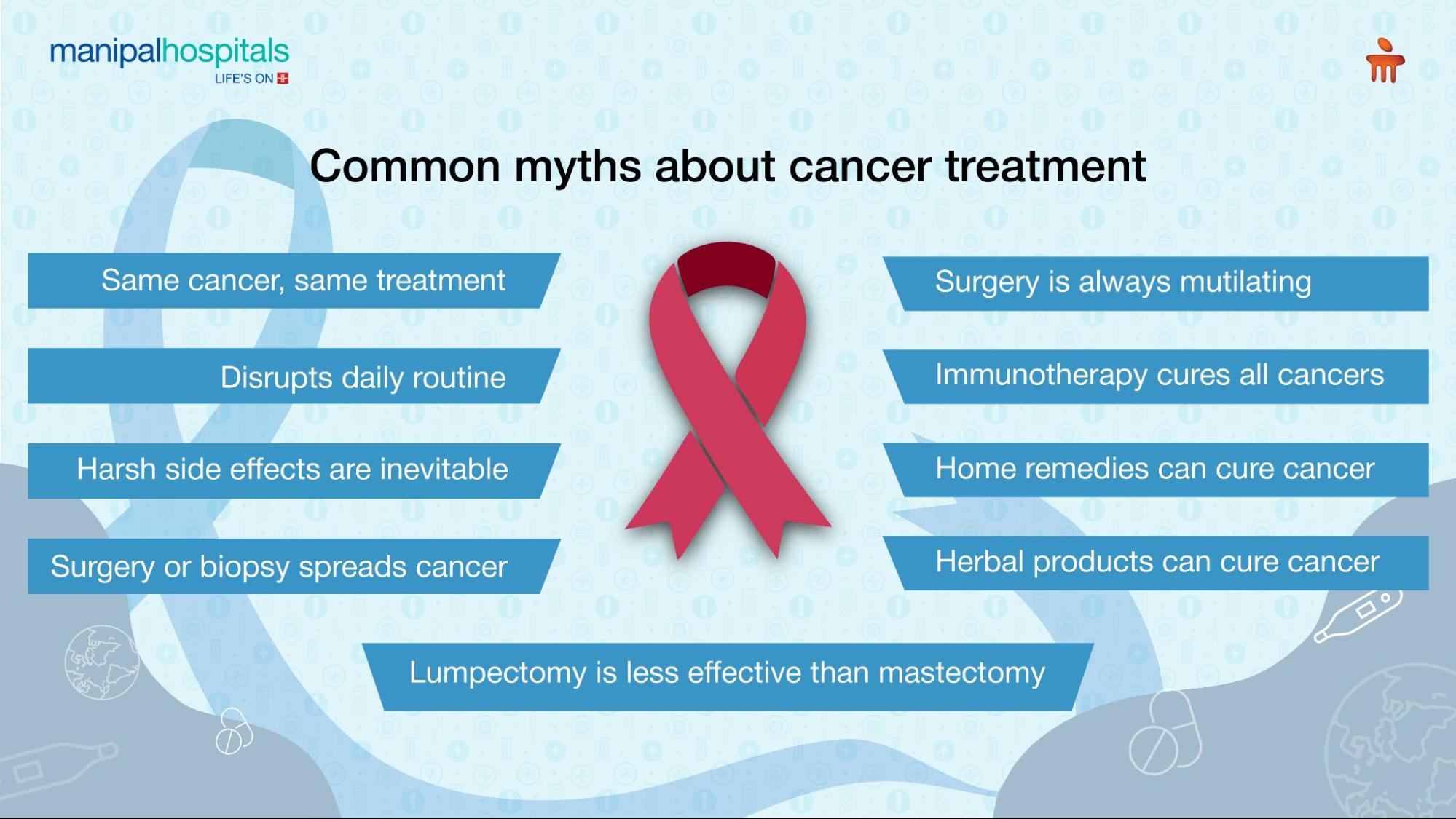
Introduction: Rethinking Cancer Myths in the Modern Era
Cancer remains one of the most intimidating health challenges we face today. With millions of people encountering a diagnosis every year, our understanding of this disease must evolve alongside technological advances and improvements in patient care. Despite remarkable progress in research and treatment, several misconceptions continue to circulate—misconceptions that can create confusing bits and tangled issues for patients and their families. In this editorial, we take a closer look at five prevalent myths about cancer that might delay diagnosis or treatment. We will also explain, in detail, why accurate, personalized information is essential for embarking on the best possible path to recovery.
Over the past 25 years, many caregivers and physicians have witnessed the nerve-racking twists and turns that come with a cancer diagnosis. Amid all the progress in modern and alternative medicine alike, it is clear that understanding the fine points of cancer care—from prevention to treatment—is super important. This article aims to steer through some of the most common misunderstandings, using clear language and reliable data, to empower patients and caregivers to find their way through the maze of information.
Personalized Treatment: Cancer Is Not a One-Size-Fits-All Disease
One of the most persistent myths is the idea that cancer is a single disease that can be treated using a standard, one-size-fits-all approach. In reality, cancer represents a group of diseases defined by abnormal cell growth, with each type displaying its own tricky parts and subtle details. Even among patients with the same basic type of cancer, genetic variability and tangled issues at the molecular level demand personalized treatment plans.
Individual Differences and the Need for Tailored Therapies
Modern research stresses that treating cancer effectively means understanding the hidden complexities of each case. For instance, studies in pancreatic cancer have shown that in more than 90 percent of cases, treatment strategies recommended by subspecialists could significantly improve patient outcomes. These findings highlight that personalized medicine is not just a buzzword but a practical, evidence-based approach that considers the little twists and turns and fine shades in each patient’s genetic makeup.
Key points in personalized treatment include:
- Detailed genetic profiling of the tumor
- Assessment of individual risk factors and lifestyle
- Collaboration among multidisciplinary teams to create tailored plans
Table: Benefits of Personalized Cancer Care
| Aspect | Traditional Approach | Personalized Approach |
|---|---|---|
| Treatment Strategy | Uniform for all patients | Custom-tailored according to genetic and lifestyle factors |
| Outcome | Varying efficacy | Improved survival and quality of life |
| Side Effects | Generalized risks | Focused management and reduced toxicity |
As we take a closer look at personalized treatment, it becomes clear that each cancer diagnosis requires an individual strategy. This approach is not only about targeting the tumor but also about understanding the subtle parts of each patient’s overall health. Medical professionals now use innovative diagnostic methods, including AI-powered assessments, to detect and target specific mutations—a strategy that moves away from old, generic protocols to finely tuned treatment regimens that consider even the complicated pieces of a patient’s biology.
Understanding Heredity: Cancer and the Role of Genetics
Another enduring myth suggests that cancer is always hereditary. Although genetic factors can play a significant role in some cases, the majority of cancers result from a mix of environmental influences and lifestyle choices. Recognizing the few small distinctions in risk factors is crucial for effective prevention and treatment strategies.
Lifestyle and Environmental Influences
Research by leading organizations, such as the American Association for Cancer Research (AACR), has shown that only a fraction of cancer cases is directly linked to hereditary factors. In the United States, nearly 40 percent of cancers have been associated with changeable risk factors. Factors such as obesity, unhealthy diets, excessive alcohol intake, and physical inactivity are driving forces that increase the likelihood of certain cancers, making lifestyle modifications a critical part of prevention.
For example, consider the following factors:
- Excess body weight: Responsible for nearly one-fifth of cancer diagnoses
- Unhealthy diet: Contributes significantly to risk, alongside obesity
- Tobacco use: Linked to around 19 percent of all cancer cases
It is essential to recognize that these environmental exposures may sometimes be unavoidable. However, awareness of these modifiable risks empowers individuals to take preventive steps. Simple changes, such as improving diet, engaging in regular physical activity, and avoiding tobacco, can help reduce the risk of developing cancer by addressing the tricky parts of daily living that contribute to tumour development.
Genetics Versus Environment: Striking a Balance
Understanding the balance between heredity and other factors allows us to appreciate the need for a holistic view of cancer prevention. While certain genetic predispositions are non-modifiable, many environmental and lifestyle factors are well within our control. This realization means that effective cancer prevention is not solely about relying on a family history of disease. Instead, it is about recognizing the full range of influences—from the fine points of our dietary habits to the subtle influences of our environment—that collectively shape our overall risk.
Prevention and Early Detection: Mitigating Lifestyle Risks
There is a common but dangerous belief that nothing can be done to prevent cancer. This myth can be particularly nerve-racking because it implies inevitability, which may deter individuals from taking steps toward early detection and prevention. In reality, numerous studies have affirmed that small, everyday choices can make a super important difference in reducing cancer risk.
Everyday Habits That Break Down Cancer Risk
Our daily habits can be the key to preventing many types of cancer. From shielding our skin from harmful ultraviolet radiation with sunscreen to making healthier food choices, each decision can either pave the way for or help mitigate the development of cancer. Here are some critical habits that can help:
- Wearing sunscreen and protective clothing when outdoors
- Choosing a balanced diet rich in fruits, vegetables, and whole grains
- Steering clear of tobacco and moderating alcohol intake
- Ensuring regular physical activity to maintain an optimal weight
In addition to lifestyle changes, vaccines have emerged as an essential component in the fight against cancer. Vaccinations against infectious agents like human papillomavirus (HPV) and hepatitis B have made a significant impact by reducing the risk of cancers such as cervical, vulvar, and even liver cancer. These preventive measures are not only practical but also represent a proactive approach to combat the onset of disease—demonstrating that while some elements may be scary, there are many ways to take control.
Technological Innovations in Early Detection
Advances in technology have introduced innovative tools that facilitate early cancer detection, making it easier for patients to get around the pitfalls of late diagnosis. Recent developments in artificial intelligence, for instance, have enhanced the accuracy of screenings such as colonoscopies, helping to identify colorectal cancer in its early, more treatable stages. Additionally, new FDA-approved technologies now enable self-collection of specimens for cervical cancer screening, which not only increases comfort but also improves adherence to screening recommendations.
These technological enhancements underscore the importance of early detection and the critical role that daily habits and preventive measures play in reducing cancer risk. They remind us that while some exposures and risks are inevitable, the more we take charge of our health, the greater our chances of catching cancer early—when treatments are most successful.
Reassessing Pain: Cancer Is Not Always Synonymous With Suffering
There is a widespread misconception that cancer always comes with overwhelming pain. This belief can lead patients to ignore or misinterpret symptoms, potentially delaying diagnosis and treatment. It is important to recognize that pain is not necessarily an early indicator of cancer. In many cases, particularly in the early stages, the disease may progress without noticeable pain.
Understanding When Pain Signals Caution
While pain is undoubtedly one of the more nerve-racking symptoms that can occur in the later stages of cancer, its absence does not guarantee that everything is fine. Especially during the early phases of some cancers, there might be few to no overt signs of discomfort. Relying solely on pain as a signal for seeking treatment can lead to dangerous complacency, ultimately allowing time for the cancer to advance unchecked.
Innovations in early detection have made it clear that recognizing other subtle symptoms and changes in the body is critical. For example, the use of AI-powered imaging technology during routine screening procedures can identify tiny irregularities that might otherwise be missed. These cutting-edge tools are designed to pick up the confusing bits and fine points of cancer’s development long before physical pain becomes apparent, thus increasing the likelihood of successful intervention.
Table: Comparing Traditional Symptom Awareness vs. Advanced Screening Techniques
| Aspect | Traditional Approach | Advanced Technology |
|---|---|---|
| Symptom Reliance | Focus on pain and discomfort | Utilizes imaging and molecular markers |
| Detection Timing | Often late-stage discovery | Early-stage detection through subtle indicators |
| Patient Outcome | Delayed treatment, reduced survival rates | Prompt intervention, improved prognosis |
This comparison highlights how early detection efforts backed by modern technology can identify issues before they progress to a stage where pain becomes the primary indicator. Therefore, understanding the little twists of how cancer manifests—and realizing that pain is just one of many possible signs—allows patients to work with healthcare providers proactively, ensuring they are not misled by misconceptions into overlooking early warning signs.
Alternative Therapies: Complementary, Not Curative, in Cancer Care
Another dangerous myth is the belief that alternative therapies alone can cure cancer without the support of standard, evidence-based treatments. While many complementary approaches may help alleviate symptoms and improve quality of life, they are not a substitute for rigorous, scientifically validated treatments. Established cancer therapies have seen rapid advancement and continue to offer real hope by effectively managing even the tricky parts and hidden complexities of the disease.
The Role of Complementary Therapies
Complementary treatments—such as acupuncture, meditation, and nutritional therapies—can be valuable in managing stress, reducing side effects, and improving overall well-being during cancer treatment. However, it is critical to remember that these treatments should serve as adjuncts to, and not replacements for, conventional medical care. The super important advances seen in modern oncology, including antibody-drug conjugates (ADCs) and immunotherapy, underline that the core treatment for cancer must be rooted in evidence-based medicine.
When considering alternative therapies, patients should:
- Consult with their healthcare team to understand how these options fit into their overall treatment plan.
- Avoid forgoing standard treatments that have been scientifically tested and proven to work.
- Use complementary therapies to manage side effects and improve quality of life, not as a standalone cure.
Adapting to New Treatment Modalities
Recent findings and approvals from the FDA underscore the essential role that traditional treatments play in modern cancer care. For example, during the period from July 2023 to June 2024, the FDA approved multiple new anticancer therapeutics and repurposed existing drugs for new uses. These advances demonstrate that cancer treatment is moving quickly, evolving with the latest scientific insights. New medications, targeted therapies, and innovative approaches—such as antibody-drug conjugates—are showing promising outcomes for patients with various types of cancer.
The progress in standard treatments serves as a reminder that while alternative therapies can be part of the overall approach to care, they are best used in conjunction with, not instead of, medically validated treatments. It is only by combining the strengths of both conventional and supportive therapies that patients can hope to overcome the tangled issues and subtle parts of cancer effectively.
Conclusion: Empowerment Through Education and Personalized Care
In the fight against cancer, dispelling myths and replacing them with clear, accurate information is key. The journey through cancer is undeniably filled with twists and turns, but with continued research, technological advances, and personalized care, patients can get around the many obstacles they may face. Understanding that cancer is not a single, homogeneous disease; that heredity is only one piece of the puzzle; that prevention through healthy lifestyle choices can make a super important difference; that pain is not always an early sign; and that alternative therapies cannot replace evidence-based treatment is essential for making informed decisions.
By taking a close look at these misconceptions, we are better able to provide guidance and reassurance during a time that is often overwhelming. Healthcare professionals, researchers, and patient advocates are continuously working to unravel the confusing bits and subtle details of cancer, ensuring that patients receive timely, personalized, and effective care.
Here is a quick summary of the key points discussed:
- Personalized Care: Effective treatment must be tailored to each patient’s unique genetic makeup and circumstances.
- Hereditary vs. Environmental: Although genetics plays a role, modifiable lifestyle factors are equally critical in developing cancer.
- Prevention through Lifestyle: Daily habits, including diet, exercise, and sun protection, are crucial in reducing risk.
- Early Detection Over Pain Reliance: Technological advances allow for early diagnosis, even when pain is absent.
- Complementary Treatments: While supportive therapies improve quality of life, they must complement, not replace, traditional treatments.
Ultimately, the battle against cancer is one that demands a balanced view—a view that acknowledges both the slight differences in individual cases and the collective importance of advancing science and technology. Patients should feel empowered to ask questions, consult with specialists, and actively work with their medical teams to craft treatment plans that address both the fine points and the broader picture of their health.
Medical advancements continue to offer hope amidst the tangled issues and nerve-racking uncertainties of a cancer diagnosis. With personalized treatment, effective prevention strategies, improved diagnostic technologies, and an informed perspective on both conventional and alternative therapies, the future of cancer care looks brighter. This knowledge-sharing is essential in helping each individual steer through the complicated pieces of their health journey, equipping them with the tools and clarity they need to fight back against the disease.
For patients, families, and caregivers alike, maintaining an open dialogue with healthcare providers and staying informed about the latest research is a must-have strategy. As more data emerge and our understanding of cancer’s twists and turns deepens, we can only hope that myths will give way to clear, factual guidance, ensuring timely diagnosis and effective treatment for all.
Looking Ahead: The Promise of Continued Research and Education
As we move forward, the importance of education in dispelling toxic myths and empowering patients cannot be overstated. Educating oneself not only helps in understanding the subtle parts and fine details of cancer but also in taking the wheel when making health decisions. Continued research in oncology and supportive fields offers fresh insights into preventing, detecting, and treating cancer. Observing the latest trials, regulatory approvals, and technological innovations highlights an ever-optimistic road ahead.
Several promising areas that deserve close attention include:
- Artificial Intelligence in Screening: Tools that analyze imaging data to catch early signs of cancer even before symptoms like pain appear.
- Immunotherapy Advancements: New methods that harness the body’s own defenses to target cancer cells more accurately and effectively.
- Genomic Profiling: Increasingly detailed genetic maps that drive personalized treatment strategies.
- Nutritional Science and Diet: Continued research into how diet and lifestyle choices affect cancer risk, prevention, and recovery.
- Innovative Preventive Vaccines: Development and wider adoption of vaccines to protect against virus-related cancers.
These developments are super important because they promise a future where the treatment paths for cancer are not only more refined but also more accessible and tailored to individual needs. With each breakthrough, the rough, intimidating aspects of the disease recede, replaced by new strategies that simplify the process of treatment and recovery.
Final Thoughts: Empowerment Through Clarity and Personalized Support
In conclusion, our journey through the tangled issues of cancer care reveals that clear, fact-based information is the cornerstone of improved outcomes. Dispelling myths—whether about the nature of the disease, its hereditary links, the role of preventative measures, the presence or absence of pain, or the limits of alternative therapies—ensures that patients and their families can make informed decisions without getting stalled by misleading beliefs.
As you work your way through the complexities of diagnosing and treating cancer, remember that every individual’s journey is unique. Embrace the advantages of personalized care, foster healthy lifestyle habits, and trust in the significant advancements that modern medicine has to offer. With continuous education, collaboration among healthcare professionals, and a commitment to clear, patient-centered communication, we can make strides in reducing the delays and challenges that cancer myths can impose.
Ultimately, this editorial is a call to action for both the medical community and patients: let us replace confusion and apprehension with facts, support, and a forward-thinking approach to cancer care. By staying well-informed and proactive in every step of the process, you can confidently take a closer look at the small distinctions that make a significant difference in your health journey.
Knowledge is power, and with the continuous advancement of research and technology in oncology, there is every reason to be hopeful. The road may be full of tricky parts and tangled issues, but with the right information and support, every patient can find their way to better health and improved outcomes. Let us all commit to debunking myths and embracing a future where informed decisions, personalized approaches, and cutting-edge treatments redefine what’s possible in the fight against cancer.
Originally Post From https://kevinmd.com/2025/06/5-cancer-myths-that-could-delay-your-diagnosis-or-treatment.html
Read more about this topic at
Common Cancer Myths and Misconceptions – NCI
Popular myths about the causes of cancer