Introduction: Weighing Your Options in Shoulder Arthroplasty
Shoulder arthritis has long been a tricky area in modern orthopedic surgery, with both patients and clinicians facing confusing bits when trying to decide between treatment methods. As advances continue to emerge in both traditional total shoulder arthroplasty (TSA) and the ream and run (RnR) technique, it is essential to take a closer look at how these options compare. This opinion editorial will explore the two procedures in detail, comparing outcomes, surgical approaches, and patient factors in a neutral discussion. Our aim is to offer an informed perspective to help guide choices in treating glenohumeral arthritis.
Treatment Options for Glenohumeral Arthritis: TSA Versus Ream and Run
Glenohumeral arthritis, or shoulder arthritis, presents several twists and turns when it comes to treatment planning. Traditionally, total shoulder arthroplasty has been the preferred method, involved in replacing both the humeral head and the glenoid with prosthetic components. However, concerns over the potential for complications—especially those related to the glenoid component—have led some patients and surgeons to explore alternative approaches, such as the ream and run procedure.
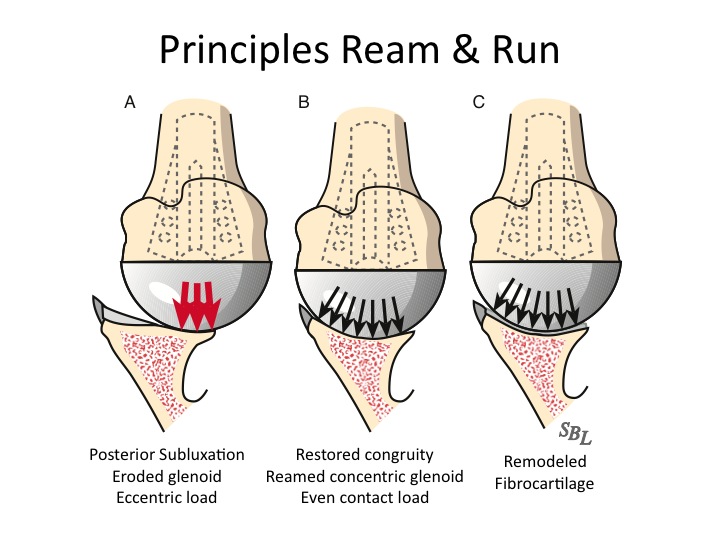
Understanding the Ream and Run Technique in Detail
The ream and run technique is a less conventional approach that avoids the use of a prosthetic glenoid component altogether. Instead, it focuses on reaming the glenoid to create a smooth surface that, with time and the right rehabilitation, regenerates fibrocartilage. This method may sound a bit intimidating at first due to its deviation from the well-trodden TSA path. However, for younger, active patients who are eager to avoid some of the long-term complications of TSA, this procedure offers a way to bypass the tangled issues associated with implant wear.
At its core, the RnR procedure replaces only the humeral head. Surgeons then reshape the glenoid bone, relying on the body’s natural healing process to form the smooth surface required for lasting joint function. This approach has caught the eye of many clinicians since it directly addresses the problematic fine points linked with prosthetic glenoid components. By avoiding that implant, the ream and run technique sidesteps many of the nerve-racking complications that sometimes arise post-TSA, such as loosening, wear, and the need for revision surgery.
Delving into Total Shoulder Arthroplasty
Total shoulder arthroplasty remains a widely recognized procedure that effectively improves shoulder pain and functionality. It involves replacing both the humeral head and the glenoid, thereby restoring joint mechanics. Although TSA is highly effective, it comes with its own set of complicated pieces, such as the risk of prosthetic glenoid loosening over time. For some patients—especially those with higher activity demands or younger individuals—the risk of early failure constitutes a significant consideration.
The interventional choices between TSA and RnR often hinge on the balancing of immediate improvements against long-term risks. TSA offers reliable early results; however, its pitfalls lie within the potential for long-term issues that may necessitate further surgery. On the other hand, while the ream and run procedure minimizes certain long-term prosthetic complications, it is not without its own potential for repeat procedures. This duality raises a key question for our discussion: how do patients and surgeons decide which approach aligns best with individual goals and lifestyle demands?
Clinical Outcomes and Patient-Reported Measures: What Do the Numbers Tell Us?
Both TSA and RnR have been shown to significantly improve patient-reported outcome measures. Important assessments include pain levels, range of motion, and overall functional scores as reported through tests such as the Simple Shoulder Test (SST) and the American Shoulder and Elbow Surgeons (ASES) score. Meta-analyses have demonstrated that, regardless of the chosen procedure, patients exhibit marked improvements postoperatively.
Breaking Down the Patient-Reported Metrics
Data shows that both groups—those undergoing TSA and those receiving RnR—experience enhancements in shoulder functionality and reduction in pain. Patients report a significant decrease in visual analog scale (VAS) pain scores, as well as gains in active forward elevation and external rotation. These improvements offer a hopeful perspective in the ongoing debate between these procedures.
Here is a summary table based on compiled studies from recent literature:
| Outcome Measure | Ream and Run (RnR) | Total Shoulder Arthroplasty (TSA) |
|---|---|---|
| Simple Shoulder Test Score Increase | Approximately 5 points | Approximately 4.5 points |
| ASES Score Increase | ~40.5 points | ~40.2 points |
| VAS Pain Reduction | ~4.08 point reduction | ~3.93 point reduction |
| Forward Elevation Improvement | ~24.75º | ~40.5º |
| External Rotation Improvement | ~21.22º | ~19.72º |
The clinical data indicate that both methods offer significant benefits. However, it is important to recognize that patient selection plays a key role. Younger patients often lean toward RnR, while older patients might prefer the tried-and-true TSA. These differences highlight the need for an individualized plan, underscoring that while the numbers are promising, they are only part of the picture.
Pros and Cons: A Closer Look at Functional Outcomes
When comparing TSA and RnR, several subtle details come into play. The following bullet points summarize the pros and cons observed in studies:
- Ream and Run (RnR):
- Allows avoidance of glenoid component complications
- May be a suitable option for physically active, younger patients
- Relies heavily on rigorous postoperative rehabilitation
- Shows a slightly higher revision rate in some studies
- Total Shoulder Arthroplasty (TSA):
- Well-established procedure with a long track record
- Offers significant improvement in pain and functionality
- Carries risk of prosthetic loosening, particularly in active patients
- May entail long-term activity restrictions to preserve implant integrity
These points emphasize that while the outcome improvements might seem similar on paper, the finer aspects—such as patient lifestyle, age, and willingness to adhere to rehabilitation protocols—can greatly influence which method is best suited for a given individual.
Patient Selection and Surgical Technique Variability
One of the more confusing bits surrounding shoulder arthroplasty is the subtle parts involved in patient selection. Not every patient is a good candidate for every procedure. Over time, researchers have identified key differences that may steer a patient toward one option over the other. With TSA being more common in older patients with lower activity demands, the ream and run technique tends to attract younger, more active individuals who are eager to avoid the potential long-term issues that come with prosthetic glenoid components.
The Impact of Age, Sex, and Lifestyle Factors
Studies show that demographics tend to influence outcomes. For instance, the ream and run cohort often comprises younger patients, who not only have higher physical demands but are also typically predominantly male. This observation may be linked to the overall selection bias, as younger patients may have the nerve-racking responsibility of enduring an intensive rehabilitation program.
It is essential to note a few key points about patient selection:
- Patients who are younger and have higher activity levels often prefer RnR for its potential longevity in active use.
- Those with a history of substance use or other comorbidities might fare better with TSA, which offers a more predictable early outcome.
- Preoperative physical condition and patient motivation are critical; the success of RnR largely depends on committing to a demanding rehabilitation process.
These considerations remind us that successful outcomes are not solely based on the technique, but also on matching the patient’s profile to the chosen procedure. In this way, selecting the right candidate for RnR can lead to a rewarding experience, though it does involve navigating through the complicated pieces of preoperative and postoperative planning.
Surgical Techniques: Handling the Subscapularis and Glenoid Reaming
Another twist and turn in the decision-making process is the variation in surgical techniques. The ream and run method, for example, shows differences in how the subscapularis is managed. Some surgeons may prefer a lesser tuberosity osteotomy, while others opt for a combined tenotomy-peel technique or a subperiosteal peel-back method. The choice of technique can influence postoperative stiffness, pain levels, and the potential for reoperation.
In contrast, TSA typically involves well-standardized procedures for implant placement. However, the hidden complexities of ensuring that the prosthetic components align properly remain a challenge. Surgeons must figure a path through these intricate details in order to maximize the longevity of the implant and minimize the risks of revision surgery.
The following table summarizes some of the key variations and their implications:
| Method | Surgical Approach | Key Considerations |
|---|---|---|
| Ream and Run (RnR) | Deltopectoral approach with various subscapularis management techniques |
|
| Total Shoulder Arthroplasty (TSA) | Standard implant-based replacement for both humeral head and glenoid |
|
Rehabilitation: The Road to Recovery and Long-Term Success
Regardless of which surgical option a patient selects, the journey does not end in the operating room. Postoperative rehabilitation is super important for achieving optimal outcomes. Rehabilitation programs for both TSA and the ream and run procedures often begin on the day of surgery, with early passive range of motion exercises designed to minimize stiffness and promote healing.
The Importance of a Robust Rehabilitation Program
One of the nerve-racking challenges patients face is the intensive rehabilitation process required after these surgeries. Particularly for RnR, where fibrocartilage formation is expected to replace the reamed glenoid surface, a patient must commit to a long-term, often two-year rehabilitation program. The degree of improvement in mobility and reduction in pain is tightly linked to consistent and active patient participation in this regime.
Here are some key factors that patients should consider when planning their postoperative rehabilitation:
- Consistency: Regular physical therapy sessions are essential to maintain mobility and strength.
- Motivation: A high level of commitment is necessary to achieve the best results, especially with RnR.
- Support: Having a solid support network can help manage the intimidating schedule of therapy appointments and exercises.
- Realistic Goals: Understanding that both procedures require time to achieve full benefits can prevent frustration during the early postoperative stage.
While TSA typically has a more predictable course, the ream and run technique demands a patient who is not only physically prepared but also mentally ready to tackle an sometimes overwhelming rehabilitation process. It is crucial to think of postoperative therapy as a central part of the overall success rather than an afterthought.
Comparing Short-Term and Long-Term Outcomes
When assessing any surgical procedure, opinions on short-term gains versus long-term durability often vary. In the case of TSA and RnR, the evidence shows that both procedures produce similar improvements in the early postoperative period. However, the higher revision rate noted in some RnR studies—although not statistically significant—cannot be ignored, particularly for younger patients who might demand more long-term durability from their shoulder function.
Many experts argue that while TSA might be more predictable in the short term, its potential for glenoid component challenges over time suggests that the ream and run approach could be a compelling alternative for those eyeing a long, active life. Even so, the decision-making process should incorporate not only the available data but also personal lifestyle considerations.
Economic and Lifestyle Considerations in Surgical Decision Making
Beyond the clinical outcomes and surgical techniques, practical factors such as cost and lifestyle impact are critical in the discussion. When patients and surgeons work together to decide on shoulder arthroplasty options, they must take into account the financial implications as well as the postoperative lifestyle that each procedure entails.
Analyzing the Financial Impact of Treatment Options
The economic side of shoulder surgery is often full of problems that go beyond direct medical costs. Patients must weigh the expense of the procedure, the potential need for future revision surgeries, and the indirect costs associated with a prolonged rehabilitation program. TSA, as a more conventional procedure, may sometimes be covered more comprehensively by insurance policies compared to the less common ream and run procedure.
Key economic considerations include:
- Initial Procedure Costs: TSA often involves higher upfront costs due to the use of advanced implant technology.
- Revision Surgery Risks: Although RnR avoids certain implant complications, a higher rate of revision surgery in some studies could drive up long-term costs.
- Rehabilitation Expenses: The extended therapy regimen required for cartilage regeneration with RnR might lead to increased therapy-related expenses.
Patients should have transparent discussions with their healthcare team about these financial aspects to ensure that their choice aligns with both their health and economic objectives.
Lifestyle Implications and Activity Level Demands
The decision between TSA and RnR also deeply interweaves with the patient’s lifestyle. For someone who is highly active and expects to maintain a vigorous routine, the ream and run option might seem attractive because it aims to avoid the implant-related long-term limitations of TSA. Conversely, TSA’s established reputation and typically reliable functional outcomes make it a go-to for patients who desire minimal disruption in their daily routines following recovery.
Consider the following lifestyle factors when making a choice:
- Activity Level: Younger, more active individuals might prefer RnR since it potentially offers better performance under high physical stress after a successful rehabilitation phase.
- Work and Recreation: Individuals whose daily activities or hobbies depend heavily on shoulder function need a tailored approach that aligns with their demands.
- Risk Tolerance: Some patients are willing to take the risk of a higher revision rate if it means avoiding the limitations associated with a prosthetic glenoid, while others may not be comfortable with that trade-off.
The interplay of these factors demands that both the patient and the surgeon work through all the complicated pieces of decision-making to determine the most suitable plan. Ultimately, the goal is to achieve a balance that minimizes pain, restores function, and supports the lifestyle the patient envisions post-surgery.
Addressing the Tricky Parts and Future Directions in Shoulder Arthroplasty
While the current body of evidence shows that both RnR and TSA offer substantial benefits, several tangled issues remain unresolved. In particular, the long-term durability of the ream and run technique continues to stimulate debate, and the slight differences in revision rates raise some nerve-racking questions for the future of shoulder arthroplasty.
Identifying Open Questions and Challenging Bits
Some of the key open questions in this debate include:
- Will long-term follow-up studies eventually show a clear advantage for one procedure over the other?
- How can surgeons better predict which patients are most likely to benefit from a rigorous rehabilitation program?
- Are there subtle differences in surgical technique that can significantly influence outcomes in a way that would sway the decision?
- What are the economic implications in the long run, considering revision rates and indirect costs?
These questions call for more extensive research, particularly large, multi-center prospective studies that delve into both the immediate and long-term outcomes of these procedures. While current data supports the efficacy of both methods, the future likely holds further refinements in surgical techniques, patient selection, and postoperative care protocols.
Future Research and Evolving Surgical Techniques
Future research should focus on the following areas:
- Long-Term Durability: Extended follow-up studies are necessary to better understand the lifecycle of both TSA and the ream and run procedure, especially in younger, active patients.
- Surgical Standardization: Efforts should be made to standardize techniques within the ream and run procedure to reduce variability in outcomes and to help clinicians figure a path through the subtle details of the operation.
- Rehabilitation Innovations: Improving postoperative therapy protocols may help mitigate some of the tricky parts of long-term recovery in both procedures.
- Cost-Effectiveness Analyses: In-depth economic studies will shed light on which procedure ultimately offers better value from both clinical and financial standpoints.
As research delves into these areas, we can expect incremental improvements that will further refine how we manage glenohumeral arthritis. Such advances will help steer through the problematic pieces of current practice, leading to more individualized and effective treatment plans.
Clinical Implications and Decision-Making: A Balanced Opinion
The available evidence clearly suggests that both TSA and the ream and run procedure offer substantial benefits in terms of pain relief and functional improvement for patients with glenohumeral arthritis. However, decision-making in this area is inherently personal and complex. Each surgical option comes with its own set of advantages and challenges, which must be weighed based on the individual’s age, activity level, and willingness to adhere to an intensive rehabilitation regimen.
Key Considerations When Choosing a Surgical Option
The following factors are super important for patients and clinicians when deciding which approach to take:
- Patient Demographics: Younger, active patients may lean toward RnR to avoid the specific issues related to glenoid implants seen in TSA.
- Surgeon Experience: The outcomes of the ream and run procedure are closely tied to the surgeon’s familiarity and comfort with the technique.
- Rehabilitation Commitment: Success in RnR hinges on a patient’s readiness to commit to a long and demanding rehabilitation process.
- Risk Tolerance: Patients must balance the immediate benefits of pain relief and improved function against the possibility of higher revision rates in the long term.
Ultimately, the decision should be made collaboratively by the patient and the medical team. Evaluating personal goals, daily activity demands, and the potential financial and emotional impact of each procedure is essential in crafting a tailored treatment plan.
Balancing Clinical Evidence with Patient Lifestyle
In the final analysis, both TSA and the ream and run technique stand as valuable options in the modern treatment landscape for shoulder arthritis. As we weigh up the data, we find that the advantages of TSA lie in its well-documented results and standardized approach, while the ream and run technique holds promise as a means to circumvent some of the confusing bits associated with prosthetic implants.
Clinicians and patients alike must work together, taking into account not just the clinical outcomes, but also the subtle details of each individual case. Such a balanced approach will ensure that the chosen treatment aligns well with both short-term expectations and long-term goals.
Conclusion: Making an Informed Choice in Shoulder Surgery
In conclusion, the debate between total shoulder arthroplasty and the ream and run approach is far from settled. Both procedures demonstrate significant improvements in pain relief and shoulder function, yet each comes with its own set of advantages, challenges, and financial implications. It is clear that no single solution fits all, and the decision-making process must incorporate a thorough consideration of patient-specific factors, including age, activity level, and willingness to engage in an extended rehabilitation program.
As this editorial has attempted to work through the tricky parts and tangled issues in shoulder arthroplasty, it is our belief that both TSA and RnR hold viable places in modern surgical practice. More extensive research and ongoing improvements in surgical techniques and postoperative care will continue to enhance our understanding and management of glenohumeral arthritis.
Patients evaluating these options should have honest discussions with their orthopedic surgeons, considering not only the technical aspects but also the impact on their lifestyle. Whether pursuing the well-established path of TSA or opting for the alternative offered by the ream and run procedure, the ultimate goal remains the same: to restore function, reduce pain, and allow patients to return to a fulfilling active life.
While the decision can seem overwhelming and even a bit nerve-racking, being informed about the subtle details—those fine points and little twists—will help everyone involved make a choice that is as personalized as it is effective. As our understanding deepens over the coming years, the hope is that more streamlined and predictable treatment pathways will emerge, making it easier to figure a clear, evidence-based path through the sometimes confusing bits of shoulder arthroplasty.
Ultimately, the choice is personal and should be made in close consultation with experienced healthcare professionals who understand the intricate balance between immediate needs and long-term outcomes. By taking the time to dig into the research, weigh the options, and commit to the necessary rehabilitation, patients can look forward to a brighter, pain-free future with improved shoulder mobility and quality of life.
This editorial invites both medical professionals and patients to keep a critical yet optimistic outlook as we continue to sort out the challenges and celebrate the successes in the evolving field of shoulder arthroplasty.
Originally Post From https://www.cureus.com/articles/339746-ream-and-run-hemiarthroplasty-versus-total-shoulder-arthroplasty-a-comparison-of-shoulder-treatments-for-glenohumeral-arthritis
Read more about this topic at
Comparison between Anatomic Total Shoulder …
Evaluation of new normal after shoulder arthroplasty