World-Class Sarcoma and Connective Tissue Cancer Care: An Opinion Editorial
In today’s rapidly evolving world of medicine, the treatment of rare cancers – particularly sarcomas and connective tissue tumors – stands as one of the most challenging yet inspiring frontiers of healthcare. International patients, who often face a long and nerve-racking quest for answers, now have access to specialized care that not only aims to extend life but also to enhance its quality. As medical professionals and concerned citizens, it is essential to appreciate how leading institutions are working through tangled issues in oncology to offer innovative and compassionate therapies.
In this editorial, we take a closer look at the insights from experts at a world-class academic center, discussing everything from the unusual subtle details of rare cancers to the critical importance of multidisciplinary care. We also examine the emotional and practical aspects of seeking treatment internationally, and how institutions are coordinating resources to help patients and their families steer through the overwhelming twists and turns of advanced cancer care.
International Rare Cancer Treatments: Innovative Approaches for Sarcoma Patients
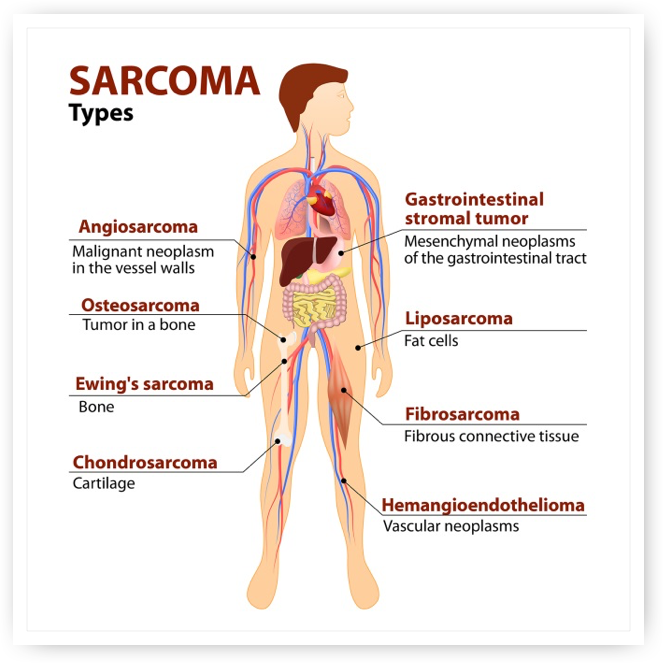
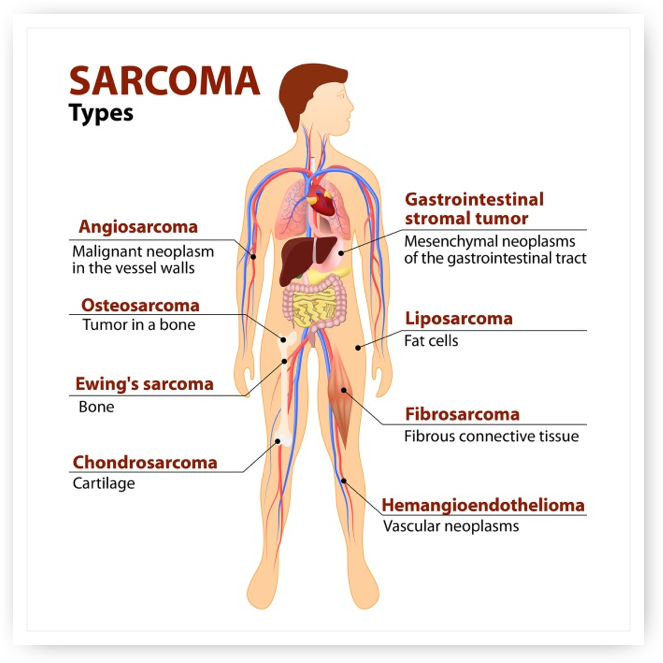
Rare cancers like sarcomas pose many tricky parts for clinicians and patients alike. These cancers include gastrointestinal stromal tumors, chordomas, desmoid tumors, tenosynovial giant cell tumors, and giant cell tumors of bone – all of which require a sophisticated approach for proper diagnosis and treatment. The rarity of these conditions often means that patients face a nerve-racking journey before finding centers equipped to manage such tangled issues effectively.
International patient care in cancer treatment is more than a matter of medical expertise; it is also about overcoming overwhelming practical challenges. From coordinating international travel logistics and explaining subtle differences between treatment plans to bridging cultural and language gaps, world-class institutions are focused on making the experience as seamless as possible. They work tirelessly to ensure that no patient feels isolated while grappling with complicated pieces of their disease.
Overcoming Tricky Parts in Advanced Sarcoma Case Management
Advanced sarcoma care is full of problems that require a very detailed and collaborative approach. When patients present with advanced or metastatic disease, the prognosis can be bleak. However, leading centers do not simply accept a fate of low survival rates; instead, they combine drug therapy, surgery, and innovative experimental treatments to offer hope. These treatments, sometimes only available at a few elite institutions globally, allow patients to access state-of-the-art procedures such as cryoablation, pulsed electric field (PEF) therapy, proton radiation, and minimally invasive, catheter-based treatments.
The practice of combining various treatment modalities is fundamental when working through the subtle parts of advanced sarcoma management. For patients who have already been told by other centers that there are no options left, discovering a multidisciplinary approach provides not only additional time but also a renewed source of hope. By integrating clinical trials into everyday practice, healthcare providers offer patients access to new therapies that may tap into the hidden complexities of cancer biology.
Addressing the Hidden Complexities of Clinical Trials in Sarcoma Treatment
Being at the forefront of research and therapy, institutions that conduct clinical trials play a super important role in shaping the future of cancer care. Running studies that go from phase 1 to phase 3 offers patients multiple avenues to explore treatments that may not be available elsewhere. These trials dive into the nitty-gritty of cancer treatment, examining combinations of drugs and therapies to produce improved outcomes for individuals with advanced sarcomas.
Clinical trials in this field are designed to address the subtle details that distinguish one patient’s journey from another’s. Although the process can seem intimidating or off-putting at first, many patients find solace in knowing that each trial is a step toward broader, innovative solutions that could benefit not just them, but future generations as well. The commitment to research in sarcoma care is a testament to the resilience of both medical professionals and patients who are committed to finding better treatment pathways.
Multidisciplinary Care: The Backbone of Advanced Cancer Treatment
One of the key factors making world-class centers so unique is their commitment to a collaborative, multidisciplinary approach. By pulling experts from surgery, radiology, pathology, orthopedics, and other fields, these institutions ensure that patients receive the highest standard of care. This model of integrated care not only tackles the tangible, challenging aspects of treatment but also supports the emotional needs of patients who may feel overwhelmed by the process.
Working through the tangled issues of cancer treatment often requires a team that collaborates seamlessly. Here is a breakdown of how multidisciplinary teams contribute to effective cancer care:
- Surgical Oncology: Experts who plan and execute intricate operations to remove tumors and reconstruct affected areas.
- Medical Oncology: Teams that manage drug therapies and coordinate experimental treatment protocols.
- Radiology and Radiation Oncology: Specialists who use advanced imaging and targeted radiation techniques to pinpoint and treat tumors.
- Pathology: Professionals responsible for the detailed analysis of tissue samples that guide treatment decisions.
- Support and Coordination: Dedicated teams who assist international patients with travel, appointments, and post-treatment care.
This integrated approach isn’t just about aggregated expertise; it is fundamentally aimed at providing personalized care that resonates with the unique circumstances surrounding each patient’s diagnosis and treatment.
International Patient Experience: Making Your Way Through a New Culture of Care
For many patients coming from abroad, the experience of seeking treatment internationally can be overwhelming. The journey is not just medically challenging but also emotionally loaded with tension and cultural differences. Transportation logistics, visa applications, language barriers, and even differing healthcare expectations can add to the nerve-racking sensation of being far from home.
At leading institutions, a dedicated international patient center works hard to streamline the process. These centers assist with everything from coordinating accommodation and travel arrangements to interfacing with local doctors for follow-up care. This comprehensive support system is designed to help patients feel at home even when they are sorting out entirely new medical and cultural contexts.
A few key aspects that international patients benefit most from include:
- Personalized Coordination: Teams that help figure a path through the administrative and practical challenges of receiving care abroad.
- Emotional and Social Support: Resources that ensure patients have access to support groups and counseling during their treatment journey.
- Global Collaboration: The opportunity for local healthcare providers to work closely with international experts, ensuring a continuum of care that extends beyond the borders of any one country.
Thanks to this level of care coordination, patients are not left to navigate a foreign healthcare system on their own; instead, they are part of a robust network dedicated to easing both the practical and emotional bit of long-term cancer care.
Innovative Advanced Therapies: Tackling the Overwhelming Challenges of Late-Stage Cancers
Advanced stages of cancer often involve a combination of daunting challenges – both for patients and researchers alike. Late-stage or metastatic cancers can be nerve-racking due to their aggressive nature and the limited time many patients have. Yet, even when facing these overwhelming scenarios, modern oncology has not shied away from exploring every possible approach.
Innovative treatments such as cryoablation, pulsed electric field (PEF) therapy, and cutting-edge proton radiation therapy have emerged as viable options for treating advanced cancers. These treatments offer a blend of precision targeting and minimal invasiveness, which, when paired with traditional surgical and drug-based strategies, provide hope for patients who might otherwise feel that all options have been exhausted.
A table outlining some modern intervention strategies is provided below to capture the essence of these advanced treatments:
| Treatment Method | Application | Key Benefit |
|---|---|---|
| Cryoablation | Freezing of tumor tissue | Minimally invasive and safe for delicate areas |
| Pulsed Electric Field Therapy | Disruption of cancer cell membranes | Potentially effective where drug resistance is seen |
| Proton Radiation Therapy | Precision radiation doses | Reduces damage to surrounding healthy tissue |
| Minimally Invasive Catheter-Based Procedures | Targeting tumors with reduced surgical trauma | Faster recovery times and fewer post-procedural complications |
The role of these treatments is growing as part of a broader initiative to offer every patient a fighting chance. Each strategy addresses a different little twist within a patient’s treatment journey, providing multiple layers of intervention that work together to combat even the most stubborn cancers.
Key Considerations for International Patients Seeking Expert Cancer Care
Patients considering treatment abroad should be ready to tackle a variety of issues that go beyond the clinical. Taking the wheel in your own healthcare journey means asking critical questions not only about your treatment options but also about the support available throughout your stay. It is super important that you understand both the medical and emotional landscape of international care before committing to a treatment plan.
Here are some practical tips for prospective international patients:
- Ask Detailed Questions: Inquire about your treatment options, including the small distinctions between various therapies and what might work best for your specific situation.
- Understand the Journey: Learn about all the steps involved, such as visa processes, accommodation arrangements, and local support systems.
- Bring Essentials from Home: Remembering tokens of home and having family or friends join, where possible, can ease the overwhelming nature of being in a foreign land.
- Coordinate with Local Healthcare Providers: Establish a clear line of communication between your home doctors and your treatment team abroad to ensure continuity of care.
Moreover, the institutions that excel in international patient care recognize that every patient’s story is unique. They work to offer not only a range of cutting-edge therapies but also a tailored support system that bridges the subtle parts of medical treatment and everyday life challenges. This attentive care is one of the main reasons that patients trust these centers when other options have fallen short.
Patient-Centered Care: Aligning Medical Expertise with Compassionate Support
The ability to pair technical medical expertise with empathetic, patient-centered care marks the true essence of advanced oncology. Here, every treatment decision is designed with the patient in mind—balancing the nitty-gritty of clinical details with far-reaching emotional support. Patients are encouraged to ask questions, express their concerns, and work hand-in-hand with their care teams to figure a path through the maze of treatment options.
In cases where the diagnosis of a rare and challenging cancer has already thrown life off balance, the added burden of figuring out treatment logistics can feel overwhelming. It is during these times that a multidisciplinary team steps in to offer guidance, making sure that each patient is afforded the same level of detailed care that would be expected at home. This supportive, hands-on approach isn’t just a nice extra—it is a must-have component of truly world-class cancer treatment.
Clinical Innovations That Are Reshaping the Future of Sarcoma Care
The rigorous pursuit of clinical innovation is at the heart of any meaningful progress in cancer treatment. New therapies, emerging research, and ongoing clinical trials are all part of a global effort to address the tricky parts of managing sarcomas and their related conditions. Academic centers lead the charge by pushing the boundaries of what is possible, ensuring that even when faced with complicated pieces of late-stage disease, patients are provided with new avenues for hope and healing.
Notably, the integration of advanced diagnostic tools, precision medicine, and personalized treatment protocols is helping to peel back the layers of hidden complexities that have, for so long, made sarcoma care a challenging puzzle. Today’s oncologists have the opportunity to dive in and test treatments that pay close attention to the little details that can mean the difference between success and setback. This ongoing commitment to research and innovation is a cornerstone for institutions that not only treat cancer but also actively search for the next breakthrough.
Expert Guidance and Transparent Communication in High-Stakes Care
An essential part of advanced cancer treatment is the relationship between patients and their healthcare teams. Clear, honest, and compassionate communication helps build trust in a process that can, at times, seem overwhelming. Medical experts who have dedicated their lives to treating rare cancers encourage patients to be proactive – to ask questions, to seek clarifications, and to understand every aspect of their treatment plan.
In a world where clinical decisions are made based on both science and experience, expert guidance provides a steady hand through the nerve-racking twists and turns of cancer treatment. Whether it is through virtual consultations or hands-on care in a state-of-the-art facility, every patient is given access to the insights and support they need to manage their disease.
Walking the International Path: A Personal Reflection on Global Cancer Care
The journey of patients seeking treatment abroad is as much about hope as it is about medical science. Each international case represents a personal battle fought against overwhelming odds. As a society, we must recognize the importance of providing not only the most advanced surgical and technological interventions but also the compassionate support necessary to lift the weight of uncertainty from patients’ shoulders.
Drawing on personal reflections from those who have experienced these challenges, it becomes clear that medical innovation and international collaboration are not mutually exclusive. Instead, they form a powerful partnership that helps individuals overcome both the confusing bits of their diagnoses and the practical hurdles of accessing global care. It is heartening to see institutions step up and offer a level of commitment that reassures patients that they are never alone on their journey.
Holistic Strategies for Managing Rare Connective Tissue Tumors
Rare connective tissue cancers demand strategies that take into account a broad spectrum of factors – from the tricky parts of medical management to the everyday challenges of living with a chronic condition. In a holistic care model, patients receive not only targeted therapies but also guidance on nutrition, mental health, and physical rehabilitation. This more inclusive approach ensures that treatment is comprehensive and effective.
Key elements of a holistic strategy include:
- Integrated Nutritional Counseling: Guidance on diet strategies that support overall health during and after treatment.
- Mental Health and Counseling Services: Professional support to help manage the stress and anxiety that often accompany a cancer diagnosis.
- Physical Rehabilitation and Fitness Programs: Tailored exercise regimes designed to increase stamina and reduce treatment-related fatigue.
- Family and Social Support: Coordination with community support groups and counseling to help loved ones cope with the challenges of care.
Through such strategies, patients learn to address both the medical and the emotional aspects of their diagnosis. They are encouraged to bring along reminders of home, engage with support networks, and develop a proactive approach to their overall well-being. These holistic elements are not mere extras—they are a super important part of what makes advanced cancer care truly effective.
Embracing the Future: How Ongoing Research Shapes Patient Outcomes
Every breakthrough in oncology is the result of persistent research and an unwavering commitment to pushing the boundaries. Advanced cancer care centers that spearhead clinical trials are not just testing drugs or procedures—they are mining the fine points of cancer biology in search of the next transformative treatment. Their work examines the little twists that lead to improved survival rates and better quality of life.
The cycle of research, testing, and innovation is both exciting and nerve-racking. It calls on researchers to take a closer look at what might have been previously dismissed as unworkable, then transforming these insights into meaningful clinical applications. For patients battling advanced sarcoma, this research is a lifeline, offering them access to treatments that are often still in their experimental stages but have the potential to turn the tide in their favor.
The benefit of this approach is twofold. Not only does the patient receive care that is on the cutting edge, but the broader medical community gains insights that help refine future treatments—creating a virtuous cycle of improvement in cancer care worldwide.
Connecting the Dots Between Research, Treatment, and Patient Advocacy
Beyond the technical and clinical aspects, there remains a critical human element in cancer care: advocacy. The voices of patients, their families, and dedicated health workers combine to create a narrative of hope and resilience that resonates well beyond the walls of any hospital. Experts in the field have long argued that quality care comes from listening to these voices, integrating their feedback into every stage of research and clinical practice.
Patient advocacy groups play a super important role in shaping research priorities and influencing healthcare policies. They shed light on the subtle details that may otherwise be overlooked in the sterile confines of scientific study. For instance, understanding the day-to-day challenges that international patients face – from language hurdles to cultural concerns – ensures that treatment protocols are not just clinically sound but also empathetically structured.
As we continue to connect these dots between research, treatment, and advocacy, it becomes clear that the future of cancer care lies in collaborative, patient-focused efforts. This approach helps to ensure that even the most advanced or intimidating cases are met with strength, expertise, and compassion.
Integrating Support Systems for a Seamless Cancer Treatment Journey
For many patients, the transition from diagnosis to treatment is filled with nerve-racking transitions and an onslaught of questions. How will they cope with the side effects? What are the financial implications? How do they plan for life after treatment? These are all questions that deserve thorough answers and empathetic guidance.
Leading institutions are increasingly recognizing that effective care requests a synchronization of medical treatment with robust support systems. The involvement of finance experts, logistical coordinators, nutritionists, and mental health professionals is key to developing a seamless care pathway. As patients work through the many twists and turns associated with their disease, these supportive services offer invaluable reassurance and practical assistance.
Below is a summary table that highlights the key components of an integrated support system for international cancer patients:
| Support Component | Description | Benefit to Patient |
|---|---|---|
| Travel and Visa Assistance | Helps with international travel arrangements and legal documentation | Reduces stress and ensures timely arrival for treatment |
| Accommodation Coordination | Arranges comfortable stays close to treatment centers | Ensures patient comfort and access to care |
| Financial Counseling | Guidance on insurance, billing, and available financial aid | Helps manage the economic aspects of long-term care |
| Emotional and Social Support | Access to counseling and support groups | Improves overall mental well-being during treatment |
Each of these components plays a key role in uniting the different bits of the treatment journey. When successfully integrated, they offer a comprehensive safety net that not only addresses the direct medical needs but also the hidden, often overlooked, aspects of patient care.
Critical Insights: Lessons Learned from Global Sarcoma Care
Reflecting on the state of international sarcoma care offers several lessons that are crucial for both patients and healthcare providers. Firstly, the need for clear, empathetic communication cannot be overstated. When patients are well-informed about all their treatment options and the support that surrounds them, the intimidating aspects of their journey become more manageable.
Secondly, the role of research in bringing fresh and effective treatment strategies is, in many ways, a beacon of hope. Constant improvements in diagnostic precision, targeted therapies, and minimally invasive procedures are a direct result of the collaborative efforts in the global oncology community. These advancements embody the spirit of embracing not only the known treatment pathways but also the promising, albeit sometimes experimental, avenues that the future holds.
Lastly, the success of international cancer care depends on the ability of institutions to adapt to the needs of each patient. No two cases are exactly alike. Some patients need extra support to figure a path through the complex bits of treatments, while others require tailored clinical strategies that address their unique disease profiles. By continuously listening to patient feedback and investing in high-quality research, healthcare providers can offer care that is both cutting-edge and compassionate.
Looking Ahead: The Future of International Cancer Treatment
As the medical community continues to explore innovative therapies and research new interventions, the landscape of international cancer care is rapidly evolving. The future promises more personalized treatment plans, improved survival rates, and increasingly integrated support systems. All these improvements point towards a future where even the most overwhelming diagnoses are met with an array of effective and humane treatment options.
Technology is playing a super important role in this evolution. Advances in telemedicine, data analytics, and precision medicine allow physicians to deliver expert advice to patients regardless of their geographic location. Virtual consultations are making it easier for international patients to get second opinions and tailored treatment plans without the initial physical travel, thereby reducing the stressful bits of the early diagnostic phase.
Furthermore, the introduction of artificial intelligence in diagnostic imaging and genetic testing is set to enhance the ability of clinicians to understand the fine points of each patient’s cancer. This means that treatments can be more precisely targeted, tackling even the slight differences between tumor types and patient conditions. As a result, the overall accuracy of treatment decisions is expected to improve, which is a promising sign for the coming years of oncology care.
Bridging the Gap: From Research Laboratories to Patient Bedsides
The journey from groundbreaking research in laboratories to tangible treatment options at the bedside is a long and sometimes nerve-racking process. However, each step of this pathway is critical and contributes to the overall success of advanced cancer care. Researchers continuously work on simplifying the tangled issues inherent in moving from experimental therapy to clinical practice, ensuring that the innovative ideas have a real-world impact.
Bridging this gap involves close collaboration between scientists, clinicians, regulatory bodies, and, importantly, the patients themselves. It requires that every new therapy is thoroughly vetted through rigorous clinical trials. Even though the process may seem loaded with problems at times, the ultimate reward is a suite of treatment options that can significantly enhance patients’ lives.
By fostering an environment where research is seamlessly integrated with clinical practice, institutions not only enhance patient outcomes but also build a legacy of continuous innovation. This collaborative spirit is what will ultimately determine the success of global sarcoma and connective tissue cancer treatment in the years ahead.
Conclusion: A Call to Action for the Global Health Community
In conclusion, the international approach to sarcoma and advanced connective tissue cancer care is a model for how high-quality, compassionate healthcare should be delivered. Patients facing intricate challenges deserve treatment that addresses both the technical and emotional twists and turns of their journey. With a multidisciplinary team that works together to manage every complicated piece of care, modern oncology is not only meeting the current demands but also paving the way for future advancements.
It is incumbent upon healthcare institutions, researchers, and patient advocates around the globe to continue working together to untangle the tricky parts of cancer treatment. By investing in comprehensive research, embracing innovative therapies, and creating robust international support systems, we can ensure that every patient, regardless of where they come from, receives the expert care they deserve.
For those of us who strive to make a difference, this evolving landscape offers a powerful reminder that hope and healing extend beyond borders. The efforts of programs and centers dedicated to treating rare cancers have already changed countless lives—and there is still much to be done. Let this editorial serve not only as an insight into the current state of advanced cancer treatment but also as a call to action for a more connected, patient-focused, and innovative future.
The journey ahead may be loaded with issues and a few overwhelming moments, but it is also filled with promise. With collaboration, compassion, and cutting-edge technology on our side, we can continue to push the boundaries of what is possible in cancer care. Every step taken by researchers and clinicians helps to clear a path for the next generation of patients—ensuring that even when faced with the nerve-racking twists of advanced disease, hope remains a constant companion.
As we look to the future, let us celebrate the progress made and reaffirm our commitment to supporting every individual battling sarcoma or other rare cancers. This global effort, intricately connected with scientific ingenuity and heartfelt care, is essential in transforming fear into strength and uncertainty into actionable hope.
Originally Post From https://www.massgeneralbrigham.org/en/about/newsroom/articles/world-class-sarcoma-connective-tissue-cancer-care-edwin-choy
Read more about this topic at
5 Innovative Soft Tissue Sarcoma Treatment Options
Sarcoma | Winship Cancer Institute of Emory University