Rural Health Investment: A Fresh Take on Equitable Funding
The announcement that hospitals in New Jersey might be eligible for a portion of the $50 billion from CMS for rural health care has sparked a lot of conversations among healthcare professionals and policymakers alike. In a discussion with CMS Administrator Dr. Mehmet Oz, State Senator Vincent Polistina outlined plans that may reshape the way rural health facilities access critical funding. This editorial takes a closer look at the opportunities and challenges involved, examines the tangled issues around eligibility criteria, and highlights the promising partnerships that could redefine medical training in South Jersey.
Examining the $50 Billion Rural Transformation Program
The Rural Transformation Program is a pivotal initiative created under the One Big Beautiful Bill Act. With this program, CMS aims to infuse much-needed capital into rural health care across the United States. For hospitals in New Jersey, the path to accessing these funds may seem overwhelming at first, but there is a clear roadmap in sight. State Senator Polistina has emphasized that some healthcare facilities in New Jersey could indeed fall under the federal designation and qualify for support.
There are several fine points to consider regarding this funding:
- Eligibility Criteria: Federal guidelines will soon lay out the exact criteria needed. For now, hospitals with limited resources and a rural status are likely to meet the necessary benchmarks.
- Funding Distribution: The funds are expected to be disbursed by the end of the year, making the next few months critical for hospitals to prepare their applications.
- Accountability and Oversight: As with any large-scale investment, keeping track of how funds are used is key to ensuring that money is spent wisely to improve patient care.
Understanding the Tricky Parts of Federal Designation
One of the most confusing bits in this process is deciphering the federal designation for rural hospitals. While new regulations are anticipated, hospitals must navigate a series of tricky parts before they can secure funding. Here are some of those challenges:
- Complex Application Processes: Hospitals need to prepare detailed documentation that showcases their eligibility. This paperwork can sometimes feel like a maze.
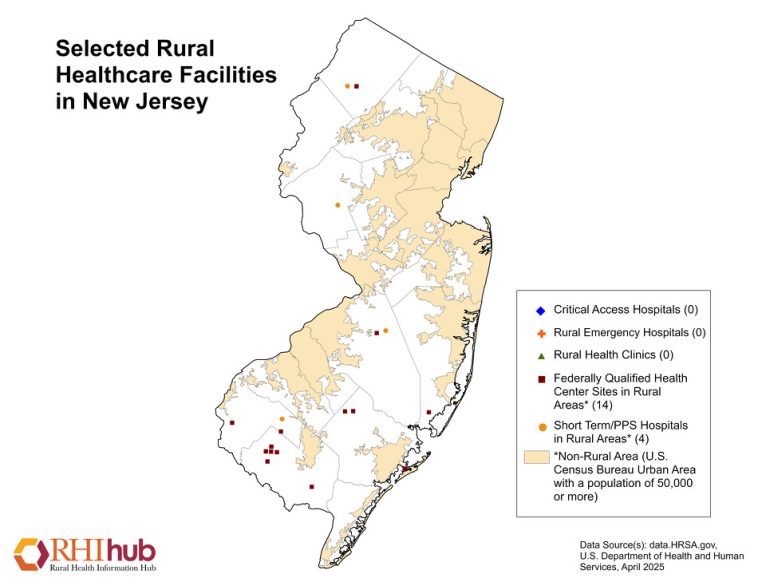
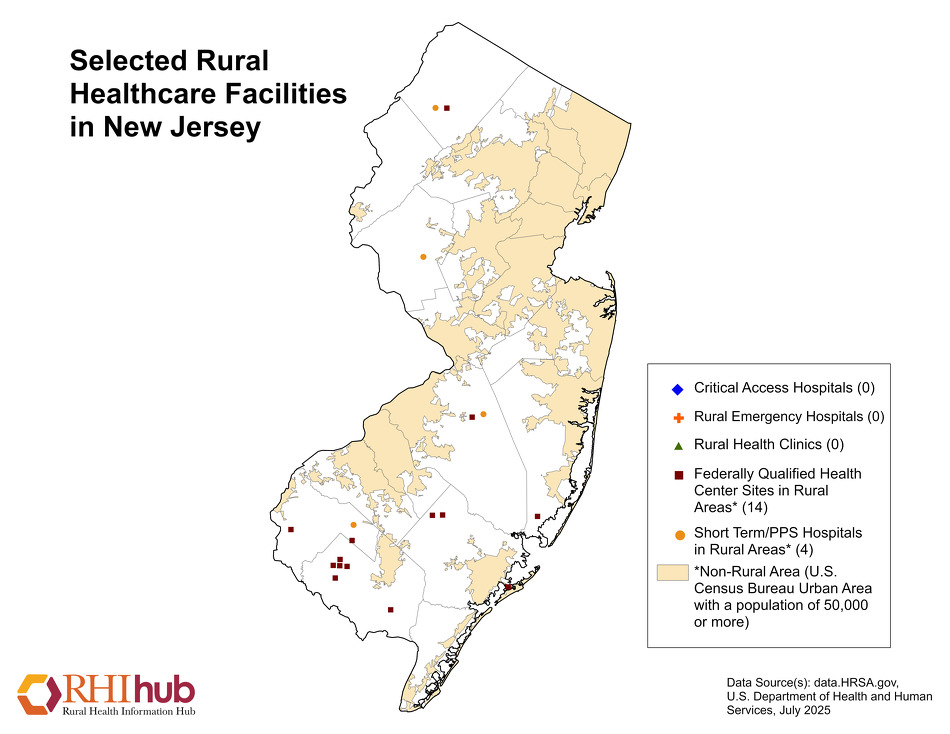
- Defining “Rural”: Determining what exactly constitutes a rural facility is another tangled issue. Geographic boundaries and population density are some of the factors being considered.
- Competition: With many hospitals across the country potentially eligible, New Jersey’s facilities must work to ensure they stand out and fully take advantage of the available funds.
Polistina’s response was both optimistic and realistic, reminding stakeholders that while challenges persist, local hospitals are well-positioned to secure a share of the funding. The state’s leadership continues to actively raise awareness about available opportunities and push for expedited guidance on the application protocols.
Enhancing Healthcare Through Strategic University Partnerships
Another exciting development emanating from New Jersey is the partnership between AtlantiCare and Stockton University, along with future associations with Drexel University College of Medicine. These collaborations are more than just symbolic gestures—they represent a strategic melding of clinical expertise and academic excellence.
From the perspective of patient outcomes, these alliances could prove absolutely essential. Here’s why:
- Local Education and Training: By establishing new medical and nursing schools in Atlantic City, the state will create a pipeline of well-trained professionals who are likely to remain in the area. This local retention is critical for building a sustainable healthcare workforce.
- Enhanced Clinical Skills: Students in these programs will be able to take part in hands-on clinical experience right in the midst of community hospitals, ensuring they understand the subtle details of rural healthcare delivery.
- Community Engagement: Educational programs often spur community-based research initiatives that address specific local health challenges, from chronic conditions to primary preventative care.
This mix of academic vigor and clinical practice is poised to help troubleshoot some of the more intimidating aspects of rural health care training. By ensuring that students not only learn theory but also gain practical experience at AtlantiCare, New Jersey is laying down a strong foundation for future healthcare professionals.
Medical Education as a Catalyst for Local Economic Growth
Investment in local educational infrastructure isn’t just important for improving healthcare—it also carries broader ramifications for regional economic growth. Training future healthcare professionals locally means that more graduates are likely to remain in the area to work, thereby reducing the outflow of talent and nurturing local expertise.
There are several key benefits to this approach:
- Job Creation: New schools and hospitals increase demand for staff, from administrative functions to specialized clinical roles. This creates multiple layers of employment opportunities in the area.
- Economic Revitalization: With an influx of educated professionals and their families, local economies experience a boost. New housing, retail opportunities, and services expand in tandem with healthcare improvements.
- Long-Term Stability: When a region develops a strong, sustainable healthcare ecosystem, it becomes more resilient in times of economic uncertainty.
Investing in education and training addresses the immediate need for skilled professionals while also planting the seeds for sustained economic and healthcare improvements in the long run. The strategic mix of sound financial planning and robust academic partnerships could very well serve as a blueprint for other states facing similar challenges.
Overcoming the Overwhelming Challenge of Healthcare Funding Inequities
Healthcare funding, especially in rural regions, can sometimes seem nerve-racking due to the many overlapping layers of bureaucracy and competition for scarce resources. Rural hospitals are often on the edge of survival without the intervention of programs like the Rural Transformation Program.
Key areas that require immediate attention include:
- Streamlining application protocols
- Clarifying the boundaries of rural designation
- Ensuring transparent distribution of funds
For many community leaders and hospital administrators, these are not just abstract policy dilemmas—they are matters that affect day-to-day operations and patient care. There is a growing sense that solving these complicated pieces may require innovative approaches and stronger advocacy from both state officials and local leaders.
Local Training Initiatives: Building a Homegrown Healthcare Workforce
The emphasis on educational initiatives in collaboration with institutions like Stockton University and Drexel University College of Medicine is a clear response to another critical challenge: the shortage of healthcare professionals in rural areas. By focusing on training local residents, the state hopes to foster a self-sustaining workforce that understands the local community’s needs.
State Senator Polistina pointed out that training programs are not just about churning out numbers—they are about ensuring quality care for the community. Consider the following benefits of locally focused training initiatives:
- Cultural Competence: Learners from the area are more likely to appreciate local customs, languages, and social norms, thereby providing care that is both respectful and effective.
- Increased Retention: When local youth are offered avenues for education and subsequently offered employment in the same region, the cycle of migration is broken, stabilizing the local workforce.
- Proximity to Care: Training done in local hospitals ensures that students are well-versed with the specific health challenges of their community, be it chronic illnesses, mental health issues, or infectious diseases.
These training initiatives offer an important counterbalance to the brain drain often observed in rural areas where talented individuals move to urban centers in search of better opportunities. By nurturing homegrown talent, New Jersey is not only strengthening local health care in the short term but securing a durable and resilient workforce for the future.
Balancing Federal Funding with State-Level Priorities
While the infusion of federal dollars offers much promise, the effective use of these resources requires a thoughtful approach that blends national priorities with the specific needs of local communities. The conversation around the $50 billion Rural Transformation Program isn’t merely about money—it’s about how best to use that money to address the small distinctions that make or break the delivery of quality health care in rural settings.
Consider these factors when balancing federal funding with state-level initiatives:
- Local Customization: Federal programs need to provide flexibility so that rural hospitals can adjust to their specific community challenges.
- Combined Expertise: Partnerships between public institutions and private healthcare systems can greatly improve outcomes by leveraging both sets of expertise.
- Monitoring and Evaluation: It is essential that each dollar is tracked and its impact measured, especially in areas with limited resources. This requires setting up systems that can flag any nerve-wracking issues early on.
Stakeholders agree that the benefits of a well-implemented federal grant program stretch beyond immediate patient care. They extend into the realms of community welfare, economic stability, and a much-needed boost to local infrastructure. These combined efforts illustrate the small twists that policymakers must consider when designing programs that aim to serve diverse and often rural populations.
Addressing Public Concerns and Tensions Around Health Care Funding
Despite the clear benefits, discussions around federal funding of rural health care can be on edge. Some community members worry about potential mismanagement, while others question whether the funds will reach the facilities that need them the most.
Common concerns include:
- Lack of Transparency: Citizens often feel that government funding schemes are riddled with hidden complexities that make it hard to know where the money is ultimately spent.
- Inequitable Distribution: There is an ongoing debate over whether funds will be allocated evenly or primarily to already well-resourced systems.
- Bureaucratic Delay: Many fear that the application and approval process might become a stumbling block, delaying much-needed improvements in care.
Addressing these issues requires an honest look at the little details involved in managing a large-scale funding initiative. It’s crucial for policymakers to engage directly with hospital administrators, local community leaders, and even independent experts to ensure that every step taken is transparent and aimed at bolstering community health.
Enhancing Communication: A Two-Way Street
One of the key factors in the success of any public health initiative is open, clear, and continuous communication between state agencies and local healthcare providers. The conversation between Senator Polistina and Dr. Oz illustrates a crucial point: funding programs are only as effective as the communication channels that support them.
Effective communication benefits the process in the following ways:
- Clarifying Application Procedures: Well-defined guidelines and easy-to-access information can help hospitals understand and satisfy federal criteria.
- Building Trust: Regular updates from federal and state officials help build community trust in the process, making it easier to implement broad-based changes.
- Feedback Mechanisms: Establishing a feedback loop ensures that any challenges are quickly addressed, smoothing out the twists and turns often encountered during complex bureaucratic processes.
Furthermore, advances in digital tools and telecommunication systems can help streamline these communication channels. The integration of modern technology into administrative processes can reduce bureaucracy, making it simpler for small hospitals to find their way through application hurdles.
Key Partnerships: Merging Healthcare and Education
The future of rural healthcare in South Jersey appears increasingly intertwined with the success of academic and clinical partnerships. The alliance between AtlantiCare and Stockton University exemplifies this point well. By linking the hands-on experience of clinicians with the latest academic research, these partnerships create a synergistic environment that nurtures innovation.
Benefits of this approach include:
- Interdisciplinary Learning: Combining different areas of expertise leads to more holistic patient care. Teachers and mentors from diverse fields help students understand subtle details involved in clinical decision-making.
- Community-Based Research: When academic institutions work side-by-side with community hospitals, research can be tailored to address local health problems directly. This allows faster implementation of new treatment protocols where they are needed most.
- Ongoing Professional Development: Continuous education for current practitioners helps ensure that the healthcare system stays updated with the latest advancements and best practices.
On a broader scale, these partnerships pave the way for innovative pilot programs that test new technologies and treatment methods. With academic institutions acting as incubators for creativity and clinical sites providing the real-world testing ground, the potential for improved healthcare outcomes in rural areas is enormous.
Policy Implications and the Road Ahead
The conversation around rural health care funding and local training initiatives is not simply a matter of short-term fixes—it carries deep policy implications for the long run. Balancing federal funds with state initiatives demands that policymakers work in close tandem with community leaders to craft regulations that are both flexible and accountable.
Some of the policy considerations include:
- Clear Guidelines: Federal agencies must issue precise and accessible guidelines for hospitals. Doing so will help local administrators figure a path through the maze of application requirements.
- Performance Metrics: Establishing measurable outcomes can help ensure that funding translates into practical benefits such as improved patient outcomes, reduced hospital readmissions, and better overall community health.
- Long-Term Commitments: Beyond one-time injections of cash, policy frameworks need to ensure that funding supports sustainable growth. This might include grants for continuous education, technology upgrades, or research projects that address ongoing community health challenges.
As policymakers continue to engage with diverse stakeholders, the focus remains on finding balanced solutions that benefit everyone. Ultimately, a coordinated approach will allow rural hospitals to thrive and help solidify the foundation upon which community health systems are built. The opportunity to turn these challenges into tangible improvements is too significant to ignore.
Real-World Impact: Voices from the Field
Patients, healthcare workers, and local residents all stand to benefit from these initiatives. In interviews and town hall meetings, many express relief at the thought of improved local care—and a sense of pride that their community is finally receiving the attention it deserves.
Some of the firsthand impacts include:
- Improved Access to Services: More funding means that hospitals can expand their services, offering everything from preventive care to specialized treatments that were previously unavailable in rural areas.
- Enhanced Quality of Care: With more resources and better-trained staff, the standard of care is expected to rise significantly, ensuring that local residents receive timely, effective treatment.
- Community Empowerment: When patients see significant improvements in public health infrastructure, a sense of community confidence grows. Local leaders are then empowered to advocate for further improvements, reinforcing a positive cycle of progress.
Feedback from frontline healthcare providers underlines that these changes are not just about numbers on a funding sheet; they touch many lives. From reduced wait times and improved diagnostic capabilities to the establishment of new clinics, the effect of strategically applied funding is both immediate and transformative.
Strategies for a Sustainable Rural Health Future
Looking ahead, what strategies will ensure that rural health care continues to improve even after the initial wave of funding? Several key elements are essential for fostering a sustainable situation:
- Community Involvement: It is super important for communities to be involved in decision-making processes. This ensures that initiatives are tailored to the specific needs and cultural contexts of the population.
- Continuous Training and Education: Establishing local training hubs will create a robust network of health care professionals who are well-equipped to tackle future challenges. This approach reduces reliance on transient staff and builds long-term capacity.
- Integrated Healthcare Systems: A seamless network of hospitals, clinics, and educational institutions can foster better coordination and continuity of care. This integration is key to addressing the many small distinctions that accumulate to determine overall quality of service.
- Regular Monitoring and Feedback: Drawing on real-time data and community feedback will help track progress, address emerging problematic issues quickly, and fine-tune strategies as needed.
In practice, these strategies might look like a dedicated committee that includes state officials, hospital administrators, educators, and even community representatives. Together, they can design action plans, set performance benchmarks, and make necessary adjustments. The table below summarizes a potential roadmap:
| Priority Area | Key Actions | Expected Outcome |
|---|---|---|
| Funding Application Guidance | Establish clear, accessible guidelines and hold training workshops | Simplified processes and higher rates of successful applications |
| Local Training Partnerships | Strengthen ties between AtlantiCare, Stockton University, and Drexel University College of Medicine | Enhanced workforce retention and improved care quality |
| Community Engagement | Organize town halls and feedback sessions | Greater public trust and more tailored care initiatives |
| Ongoing Evaluation | Implement performance metrics and analytics systems | Timely interventions and adaptive policy refinements |
This structured approach can help ensure that every aspect of the funding—be it educational improvements, infrastructural upgrades, or service expansions—are executed efficiently and with maximum impact.
Looking Forward: Optimism Amidst Challenging Turns
In many ways, the path ahead is both promising and filled with complicated pieces. There is an undeniable excitement in the air as stakeholders across New Jersey brace themselves for transformative changes in their healthcare landscape. Yet, like any major governmental initiative, there remain nerve-wracking uncertainties that must be tackled head-on.
While the policy environment continues to evolve, one fact remains clear: local communities are eager to see positive change. By taking a closer look at the funding guidelines, stepping up community partnerships, and leveraging local educational assets, New Jersey is poised to be a leader in rural health care transformation.
Consider the following key messages emerging from recent discussions with state officials and healthcare leaders:
- Empowerment of Local Hospitals: Institutions must proactively prepare and coordinate to secure their share of the funds.
- An Emphasis on Local Talent: New educational partnerships could revolutionize medical training, ensuring a homegrown workforce.
- Transparent and Accountable Implementation: Stakeholders need to work together to make sure every public dollar has a tangible impact on patient care.
These messages highlight that while the twists and turns of healthcare funding can be overwhelming at times, resilience and teamwork remain the cornerstones of progress. Every stakeholder—from hospital administrators to local students—has an important role to play in turning the promise of federal funding into real, lasting improvement in patient care and community well-being.
Final Thoughts: Charting a Path Through the Maze
As New Jersey charts its path towards harnessing $50 billion of federal support for rural health care, the focus on local training and education emerges as a critical component of the broader strategy. The intertwined relationship between academic institutions and healthcare providers enriches the quality of care available while ensuring that the pipeline of talent remains robust. In this way, the state is not just investing in short-term fixes, but in the future of healthcare itself.
In summary, the following points capture what we have learned from recent discussions and policy announcements:
- The federal Rural Transformation Program offers a unique opportunity to address long-standing challenges in rural health care.
- Enhanced partnerships between healthcare providers and academic institutions are set to improve training, patient care, and local economic growth.
- Despite nerve-wracking hurdles like complex application processes and competition for funds, proactive measures can help local hospitals secure critical support.
- Transparent communication, clear guidelines, and ongoing monitoring are super important for ensuring that every layer of this initiative succeeds.
Ultimately, while the road ahead may be loaded with challenges and occasional setbacks, New Jersey’s proactive stance and commitment to working through each stage of the process signal a bright future for rural healthcare. Leaders, policymakers, and community members alike have hopped on board with a vision that is equal parts ambitious and pragmatic. By investing in both infrastructure and education, the state is setting a high standard for holistic, community-centered care that adapts to both the immediate and long-term needs of its residents.
Conclusion: A Collective Responsibility for Community Health
The evolving landscape of rural health care in New Jersey serves as a reminder that addressing community needs is a collaborative effort. From detailed funding applications and academic partnerships to constant dialogue among stakeholders, success depends on everyone finding a way to contribute—from local hospital administrators to state senators.
This opinion editorial underscores the importance of not only seizing funding opportunities but also embracing the responsibility of nurturing homegrown talent. As South Jersey continues on this promising path, the values of clear communication, strategic planning, and community engagement will pave the way for a future where every hospital, every clinic, and every patient benefits from comprehensive and sustainable health care improvements.
In the end, the journey to better rural health care isn’t about a single program or initiative—it’s about the collective will to turn challenging twists and turns into opportunities for long-lasting, life-changing progress. As New Jersey moves forward, it is our hope that the lessons learned here will serve as a roadmap for communities across the country, reaffirming that when the local meets the federal, the benefits to public health are both far-reaching and profound.
Originally Post From https://www.ajmc.com/view/rural-health-investment-local-training-are-priorities-for-south-jersey-state-sen-vincent-polistina
Read more about this topic at
The One Big Beautiful Bill is a Historic Investment in Rural …
Rural Funding & Opportunities