Assessing the Impact of a Sweeping Tax and Spending Package on Opioid Treatment
The recent signing of a sweeping tax and spending package by the Trump Administration has ignited serious debates among public health professionals and policy experts. Some researchers warn that the new law, often referred to as Trump’s “Big Beautiful Bill,” could inadvertently lead to a loss of access for thousands of Americans who rely on opioid treatment services. In this opinion editorial, we take a closer look at the policy’s potential consequences, focusing on its effects on Medicaid, and explore the opinions of experts working to mitigate the fallout in treatment and public health initiatives.
Experts caution that while the intentions behind the legislation may have included broad economic aims, its unintended impact, particularly on medically vulnerable populations, is a pressing concern. At its core, the law is projected to strip many individuals of the health insurance they count on to obtain critical treatments for opioid use disorder. In a nation already grappling with the opioid crisis, this development has stirred a debate filled with tricky parts and subtle details that deserve a careful evaluation.
How Medicaid Cuts Could Create a Crisis in Opioid Treatment Access
One of the central issues raised by public health advocates is the predicted loss of Medicaid coverage for millions of Americans over the coming years. According to estimates by the Congressional Budget Office, as many as 7.8 million people could lose their Medicaid coverage by 2034. This scenario is particularly dire for those individuals who depend on Medicaid for life-saving medications used to treat opioid use disorder.
Projected Losses: Understanding the Scale
The analysis suggests that the legislative changes could lead to around 156,000 people losing access to opioid treatment. Based on previous studies, researchers have used simulation modeling to suggest that these losses could translate into approximately 1,000 extra overdose deaths yearly. Such projections are not merely statistics; they represent human lives caught in a shifting landscape of health policy and public health intervention.
It is essential to acknowledge that the model estimates are likely conservative. The analysis primarily centers on the inability of individuals to access medications for opioid use disorder. It does not fully account for other potential health complications—ranging from infections to heart attacks—which could further exacerbate the overall public health crisis.
What Loss of Treatment Means for Patients
The ramifications of losing access to preferred treatments are significant. For many patients battling opioid addiction, consistency in medical care is not just important—it’s critical. When patients are forced to switch to alternative medications they are less comfortable with, the effectiveness of the treatment might decline. This shift can lead to a host of issues, including treatment discontinuity, an increased likelihood of relapse, and an overall decline in patient well-being.
Here is a bullet list that summarizes the risks associated with Medicaid cuts in opioid treatment:
- Interruption and discontinuity in opioid treatment programs
- Potential increase in overdose deaths due to inadequate treatment
- Forced transitions to less effective or unfamiliar therapies
- Greater overall health complications beyond addiction
- Increased burden on public health resources for emergency care
Each of these points highlights a part of the troubled landscape created by the policy’s impact. With fewer people receiving the right kind of treatment consistently, we may see a ripple effect that leads to additional public health and economic challenges down the road.
Policy Decisions and Their Broader Public Health Implications
Policy matters are rarely isolated from larger societal issues. The predicted overhaul of Medicaid not only affects the availability of opioid treatments—it also touches upon broader elements that influence the overall health of a nation. Public health specialists argue that recent declines in overdose deaths have been achieved through very deliberate initiatives: investing in treatment options, expanding therapy accessibility, and reducing stigma attached to seeking help.
Successes from Previous Public Health Measures
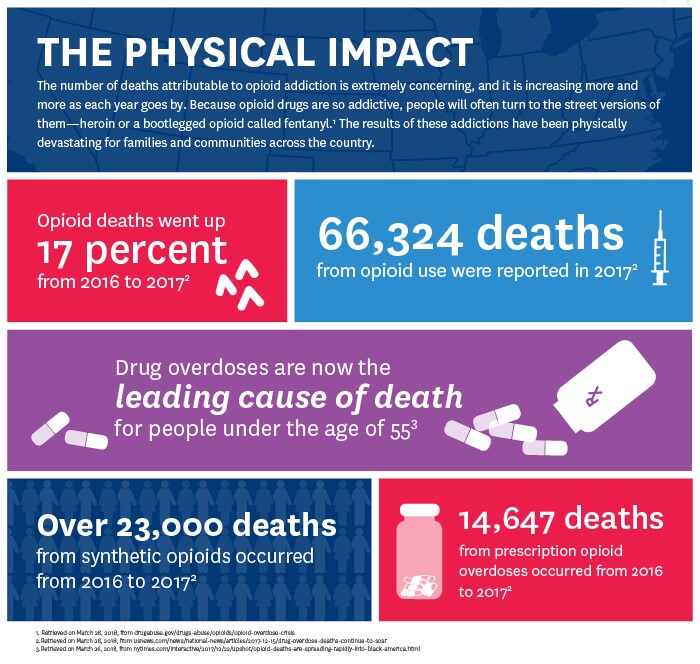
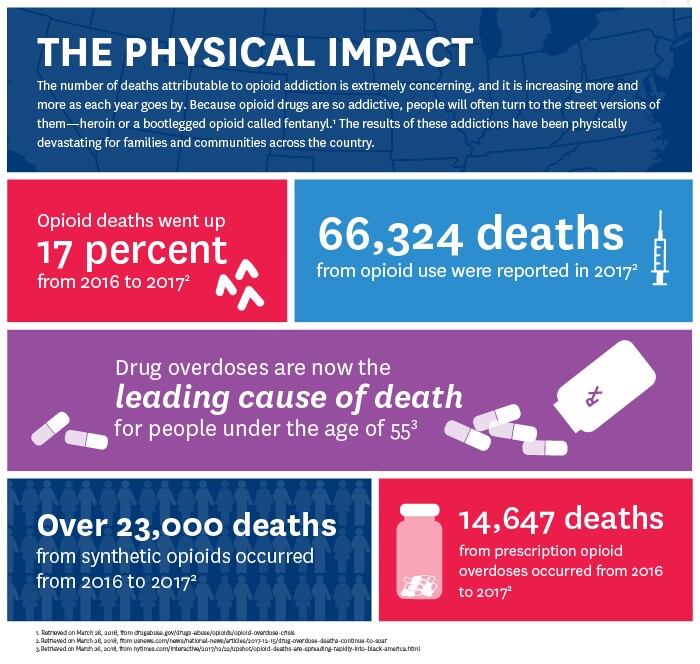
Recent data from the U.S. Centers for Disease Control and Prevention (CDC) shows a nearly 27% decline in overdose deaths from 2023 to 2024. This improvement was credited to targeted public health initiatives. Since President Trump first declared the opioid epidemic a public health emergency in 2017, investments in health services and enhanced treatment programs have yielded positive results. These results are often measured in lives saved and communities strengthened.
The success of these public health interventions emphasizes how delicate the balance is between cutting-edge treatment accessibility and the possible interruption caused by sudden policy shifts. The researchers behind the memo warn that dismantling or undercutting these foundations could easily reverse the progress we have celebrated over recent years.
Comparing the Strategies: Public Health Interventions vs. Enforcement Approaches
Notably, the Trump Administration’s approach to the opioid crisis has seen a mix of public health and enforcement strategies over time. While early efforts were focused on bolstering treatment programs, recent proposals have leaned more toward aggressive cuts to addiction treatment and research programs. This policy mix has created an environment that some experts consider to be counterproductive, emphasizing enforcement rather than supporting recovery.
The difference between these approaches can be summarized in the following table:
| Approach | Focus | Results |
|---|---|---|
| Public Health Initiatives | Investments in treatment, expanding access, reducing stigma | Decline in overdose deaths, improved patient outcomes |
| Enforcement and Cuts | Reducing spending on treatment, aggressive law enforcement | Potential increase in overdose deaths, treatment discontinuity |
It is this table of contrasts that drives home a critical point: once public health measures start paying dividends, any major policy reversal can have profound and widespread effects. The debate thus hinges on finding a balance between fiscal policy and reliable healthcare delivery.
Expert Opinions on the New Legislation
Among those voicing concerns is Dr. Benjamin Linas, a professor of medicine and epidemiology at Boston University, who led the research effort estimating the future indirect costs of the law. Dr. Linas expresses a profound worry—not just about numbers on a page, but about the very real human impact. His observations underline that when patients cannot get the treatment they know and trust, the effectiveness of even the best medications is compromised.
What Do Health Experts Believe?
Several health specialists and addiction treatment leaders have weighed in on the effects of the policy. For instance, Dr. Stephen Taylor, the President of the American Society of Addiction Medicine (ASAM), notes that while the policy’s impact might vary state by state, the basic findings regarding the reduction in opioid treatment coverage are sound. He points out that the bill contains some provisions for people with substance use disorders, such as waiving work requirements in some cases. Yet, he warns that such measures might not be enough to offset the overall risk posed by the cuts.
Here is a breakdown of the key expert opinions:
- Dr. Benjamin Linas: Believes that the additional 1,000 projected overdose deaths yearly is likely an understatement, as it does not address other severe health complications that may arise from the loss of health insurance coverage.
- Dr. Stephen Taylor: Suggests that state-level variations might alter the immediate effects of the bill but agrees that the proposed changes, if fully implemented, point to a significant potential loss of treatment accessibility.
- Public health advocates: Stress that any rollback of measures that have proven successful in reducing overdose deaths could destabilize years of progress in the fight against opioid addiction.
While expert opinions vary slightly in focus, the consensus underscores the potential human cost. The discussion is less about political leanings and more about ensuring that every individual battling addiction retains access to the critical treatments that support their recovery journey.
Exploring the Broader Economic and Social Effects
The conversation around the tax and spending package isn’t isolated to health outcomes alone. There are considerable economic and social implications that add layers to the debate. Removing Medicaid coverage from millions does not merely disrupt individual treatment programs—it also affects families, communities, and the broader economic productivity of the nation.
Economic Consequences of Losing Medicaid Coverage
If the projections hold true, and millions lose their health insurance, the economic implications extend well beyond personal healthcare. The loss of insurance coverage can lead to increased medical costs in emergency care, a higher burden on community health organizations, and a potential rise in uncompensated care costs for hospitals. As the number of uninsured grows, so too will the strain on the overall healthcare infrastructure, potentially leading to higher insurance premiums for those who remain covered.
This situation creates a set of challenging economic questions:
- What financial burden will fall on both public hospitals and private practices?
- How will communities absorb the shock of increased emergency care dependency?
- Will employers face pressure to provide more comprehensive health benefits as public coverage declines?
These questions point to intricate layers of economic stability that are interlinked with public health outcomes. Finding a pathway through this contentious policy change requires not only clear insight into the immediate shock waves but also a comprehensive strategy to mitigate long-term economic impacts.
Social Ramifications and Community Impact
Beyond the statistics and economic forecasts lie the very real stories of affected communities. When individuals lose access to essential treatments, families, neighborhoods, and entire communities feel the repercussions. The social fabric of these communities can start to fray under the pressure of untreated addiction, increased crime, and the stigma attached to substance use disorders.
Some notable social effects include:
- The emotional toll on families who lose loved ones to overdose or chronic illness.
- Increased stress on community support systems such as local clinics and charity organizations.
- The potential for social isolation among those who feel marginalized by the loss of affordable health care.
Efforts to sustain public health improvements must therefore consider these social implications. Support networks, both formal and informal, are the bedrock upon which recovery happens, and any policy that weakens these networks may inadvertently harm vulnerable populations even further.
Balancing Fiscal Responsibility with Health Priorities
The tax and spending package, sometimes celebrated as a step toward economic reform, illustrates the constant tug-of-war between fiscal responsibility and health priorities. On one side of the debate, some policy makers emphasize the need for reduced government spending, advocating that the cuts will lead to improved financial discipline and efficiency in public programs. On the other side, health experts stress that reducing funding for critical treatment programs risks reversing the hard-earned progress made in reducing overdose deaths.
Understanding the Trade-offs
When we consider the trade-offs underscored by this policy, a few key issues emerge:
- Fiscal Discipline: Proponents argue that trimming expenditures is essential for long-term economic stability. They believe that reformed spending protocols could lead to a leaner but more efficient government.
- Public Health Security: Critics counter that the stability of public health networks is equally important. They underscore the fact that lives are at stake when access to treatment for conditions such as opioid use disorder is threatened.
This dichotomy creates a tension that is both confusing and complicated. It poses the question: How does one ensure that financial reforms do not come at the expense of human health and well-being? It is a question that calls for a debate laden with twists and turns, where every decision carries both economic and human consequences.
A Roadmap for Harmonizing Policy Goals
It is possible to reconcile these two sides of the debate through a carefully structured policy framework. Decision-makers could consider targeted cuts that do not disproportionately affect those who rely on Medicaid for essential health services. Policy architects might steer through the following strategies:
- Implementing gradual changes: Phasing out cuts over time may give individuals and healthcare providers a chance to adjust without being abruptly deprived of critical services.
- Enhancing support programs: Even as cost-saving measures are deployed, robust community health initiatives and state-level programs could help bridge any gaps in treatment access.
- Monitoring and evaluation: Clear benchmarks and continuous evaluation processes can help identify when policy adjustments are necessary, ensuring that any negative impacts are swiftly addressed.
A table summarizing these strategies might look like this:
| Strategy | Potential Benefits | Challenges |
|---|---|---|
| Gradual Implementation | Smoother transition, reduced shock to systems | Requires long-term planning and coordination |
| Enhanced Support Programs | Better patient outcomes, strengthened community networks | Additional funding and resource allocation are necessary |
| Continuous Monitoring | Early detection of adverse effects, policy agility | Need for robust data collection and analysis systems |
The challenge lies in finding the right balance—a path that allows for fiscal responsibility without pawning off public health on the altar of cost-saving measures.
Looking Ahead: The Future of Opioid Treatment in an Ever-Changing Landscape
The current debate offers us an opportunity to reflect on the broader issues that underpin our approach to healthcare policy. The opioid crisis is a multifaceted challenge that demands thoughtful solutions rather than knee-jerk policy reversals. Moving forward, it is essential for policy makers, healthcare professionals, and community advocates to work together to safeguard the progress made over recent years.
Strategies for Sustaining Treatment Access Amid Policy Changes
There are several proactive steps that can be taken to ensure that vital treatments remain accessible, even in the face of sweeping policy changes:
- Building resilient healthcare systems: Focus on creating healthcare infrastructures that can adapt to shifting policies by diversifying funding sources and strengthening local partnerships.
- Advocacy and community engagement: Empower communities to advocate for their health needs, ensuring that the voices of those directly affected are heard in policy discussions.
- Investing in preventive care: Emphasizing early intervention and preventive measures can reduce the overall burden on the healthcare system and lead to better long-term outcomes.
Each of these steps represents not merely a reaction to policy changes but a broader commitment to protecting public health. They also reflect the ongoing need to find your way through an increasingly tangled policy environment, one that is loaded with issues yet demands a focus on human well-being.
The Role of Research and Data-Driven Decisions
Many of the projections discussed here arise from detailed research and simulation modeling. The reliance on data-driven approaches to predict outcomes such as additional overdose deaths is a reminder that comprehensive assessments are critical in policy-making. Researchers utilize available data on Medicaid enrollment, treatment adherence, and overdose mortality rates to model future scenarios. While these models cannot capture every subtle issue, they serve as a critical compass to help policy makers figure a path in turbulent times.
Key areas where research can further aid policy development include:
- Enhanced data collection: Continual gathering of data related to treatment outcomes and Medicaid coverage can lead to more responsive policies.
- Adaptive policy frameworks: Policies that adapt based on ongoing findings help in managing your way through an ever-evolving healthcare landscape.
- Interdisciplinary approaches: Integrating insights from economics, public health, and social sciences can lead to more comprehensive and effective solutions.
Such robust data utilization not only provides a clearer picture of the current situation but also helps to anticipate and mitigate potential future pitfalls.
Reflecting on Governance and Its Ripple Effects on Public Health
The controversy surrounding the tax and spending package is not solely about numbers—it’s also a reflection of broader governance challenges. Critics argue that the decision to implement sweeping Medicaid cuts, while intended to address fiscal concerns, may be emblematic of a larger trend in how the current Administration is governing. For those working on the front lines of healthcare, these policy reversals can feel like steps backward after significant progress has been made in the battle against the opioid crisis.
Leadership, Accountability, and Health Policy
While the policy itself is a subject of heated debate, there is an equally important conversation to be had about accountability and leadership. The health of a nation depends on decisions made by those in power, which must weigh both immediate economic constraints and the long-term health consequences for millions.
Dr. Linas and other experts point to the following challenges that highlight the tension between governance and public health:
- Policy reversals: Abrupt shifts in policy can dismantle long-established health programs, leading to confusion and reduced treatment efficacy.
- Lack of comprehensive planning: Critics argue that certain decisions seem to neglect the small distinctions in patient care and community support that are key to treatment success.
- Suboptimal focus on public health: Concentrating efforts solely on fiscal realignment without retaining essential health investments may prove to be a shortsighted strategy.
By recognizing these issues, policy makers and public health advocates are in a better position to demand leadership that not only considers budgetary targets but also recognizes the human and community costs of sudden changes.
Voice of the People: Community Concerns and Advocacy
Community voices play a crucial role in shaping public health strategies. The experiences of people who have battled opioid addiction—and their families—bring a human visage to the abstract numbers and charts. Their stories become a powerful plea for policies that bridge the gaps in treatment access and ensure that progress is not undone by political maneuvers.
Some common concerns voiced by affected communities include:
- Uncertainty surrounding continuing access to their preferred medication and treatment options.
- An overall sense of abandonment when policy changes seem to deprioritize the health of the most vulnerable.
- Frustration with shifts toward enforcement and away from community-based support and recovery programs.
Public forums, town hall meetings, and advocacy groups have emerged as critical platforms where these issues are discussed. The ongoing advocacy is a reminder of the interconnectedness of health policy decisions and the day-to-day realities of those living with addiction.
Conclusion: A Call for Collaborative and Compassionate Policies
Few policy debates are as loaded with both economic and health implications as the debate surrounding Trump’s “Big Beautiful Bill.” While fiscal responsibility is essential, it must not overshadow the critical need for accessible, effective treatment for opioid use disorder. The projections indicating 1,000 additional overdose deaths per year are not just statistics—they are warnings that without careful, measured policy decisions, progress hard-won on the public health front could be rapidly undone.
In these tense times, it becomes super important for lawmakers, health care providers, economists, and community advocates to come together. The aim should be to devise strategies that balance the need for budgetary discipline with the equally key necessity of safeguarding lives through consistent and quality health care.
The road ahead is riddled with problems and little twists that demand a nuanced approach to policy-making—one that is both data-driven and empathetic. Governance in this context is not just about managing state finances; it’s about ensuring that every citizen, especially the most vulnerable, has access to the treatments they need to lead healthier, happier lives.
Ultimately, the debate on Medicaid cuts and opioid treatment reflects a larger, ongoing conflict within public policy. As we move forward, we must work to build resilient healthcare systems that can adjust to changing policies without sacrificing the quality of patient care. Only then can we truly claim progress in both economic and health sectors, ensuring that every policy decision is as much about human lives as it is about numbers.
This editorial invites readers from all walks of life—policy makers, healthcare professionals, community advocates, and concerned citizens—to join in a dialogue. By asking critical questions, exploring the fine points of health policy, and working collaboratively, we can help steer a course that honors both fiscal responsibility and, more importantly, the lives and well-being of millions who depend on continuous health care access.
In closing, while the challenges ahead may seem overwhelming and the pathway forward may be tangled with heated debate, the commitment to protecting public health remains non-negotiable. Let us all advocate for policies that do more than just crunch numbers; let us push for thoughtful, humane, and sustainable approaches that consider every individual’s right to quality health care.
Originally Post From https://time.com/7305489/trump-big-beautiful-bill-opioids-overdose-deaths/
Read more about this topic at
National Helpline for Mental Health, Drug, Alcohol Issues
Overdose Prevention Strategy